COVID-19 Outlook: Holiday Peaks Begin to Subside
With data once again reliable enough to input into our models, we’re back this week with COVID-Lab projections to help communities interpret a very difficult phase of this pandemic. We continue to provide four-week case incidence projections, and we’re working to add new state-level forecasts for hospital admissions and census, recognizing the importance of understanding hospital trends as the nation begins to recover from the omicron wave. We hope to debut those in the coming weeks. Fortunately, our models suggest that many areas are moving past peak in case incidence, and declines in admissions and hospital census are therefore soon to follow. This is welcome news, especially for schools looking to regain footing.
Let’s first take a look at the updated case incidence data:
- Community transmission is still fairly widespread across the 812 counties included in our model; the average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) was 1.79 last week and average weekly incidence exceeded 1,000 weekly cases per 100,000 residents.
- PCR testing positivity increased, on average, from 24% last week to 31% this week, however, 1 in 6 counties saw test positivity decline in this period, up from 1 in 25 the week prior.
- As omicron transmission has become widespread throughout most of the country, our models show case incidence is peaking in most counties. The estimated time to peak varies across regions, with areas across the northern rim of the country and westward lagging just a few days to a couple of weeks behind the recovery happening in the Northeast and Mid-Atlantic.
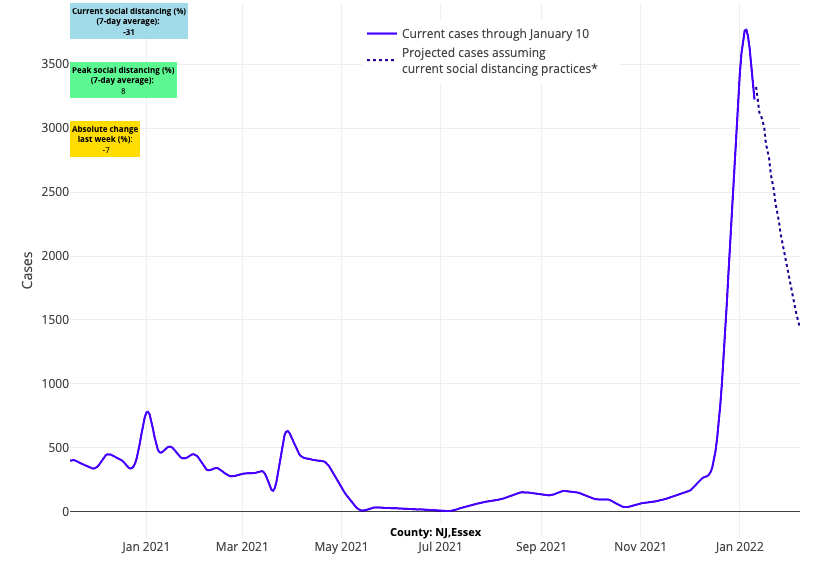
Above are the projections for Essex County in New Jersey.
- Our models show case incidence improving most quickly over the next four weeks along the I-95 corridor between New York City and Washington D.C., as well as across the I-80 corridor from Ohio into Pennsylvania.
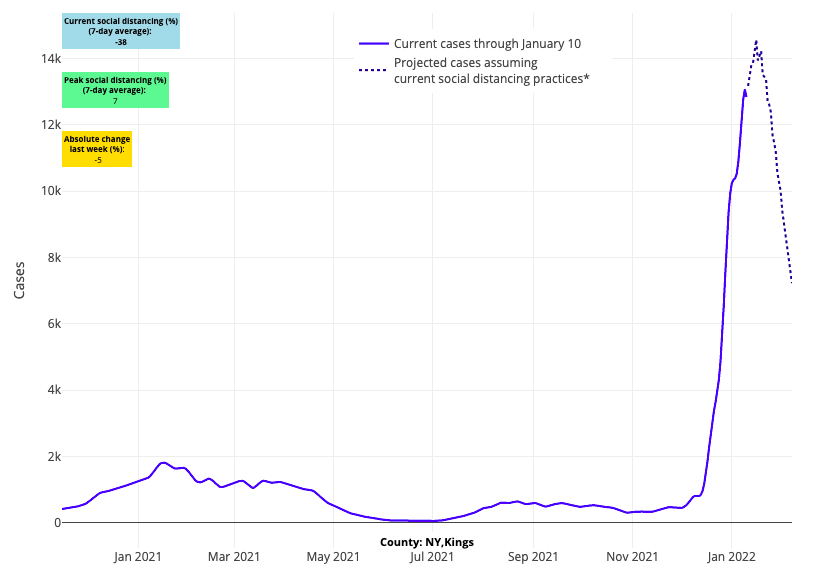
Above are the projections for Kings County (Brooklyn) in New York.
Updates on emergency department visits and hospitalizations:
- Daily hospital admissions surpassed 25,000 this past week, and adult hospital census exceeded 140,000 patients, topping peaks many regions saw last winter. Pediatric hospital census appears to have peaked around 4,800 children but has begun to fall; daily admissions have declined in the last few days from 1,600 to fewer than 1,400 children.
- This past fall, adult hospital census reached as high as 60 hospitalized patients per 100,000 residents in some states (e.g., Michigan). Many states—including Delaware, New Jersey, Ohio, New York, Illinois, Connecticut, Pennsylvania, Maryland and Missouri—are currently seeing hospital censuses exceeding that fall peak.
- States with the most rapidly increasing hospitalizations (more than 50% in the last week) include Florida, Alabama, California, Louisiana, Mississippi, South Carolina, Georgia, Washington, Texas and Hawaii.
- Over the last few days, the Northeast and Mid-Atlantic regions have seen declines of 20% or more in adult admissions, particularly in counties across New York and New Jersey. This has been accompanied by declining emergency department visits that are nearly half of what they were between Christmas and New Year’s. Similar reductions in emergency department visits are occurring from Philadelphia down through Washington, D.C., and into Virginia, where declining admissions may be just a few days behind.
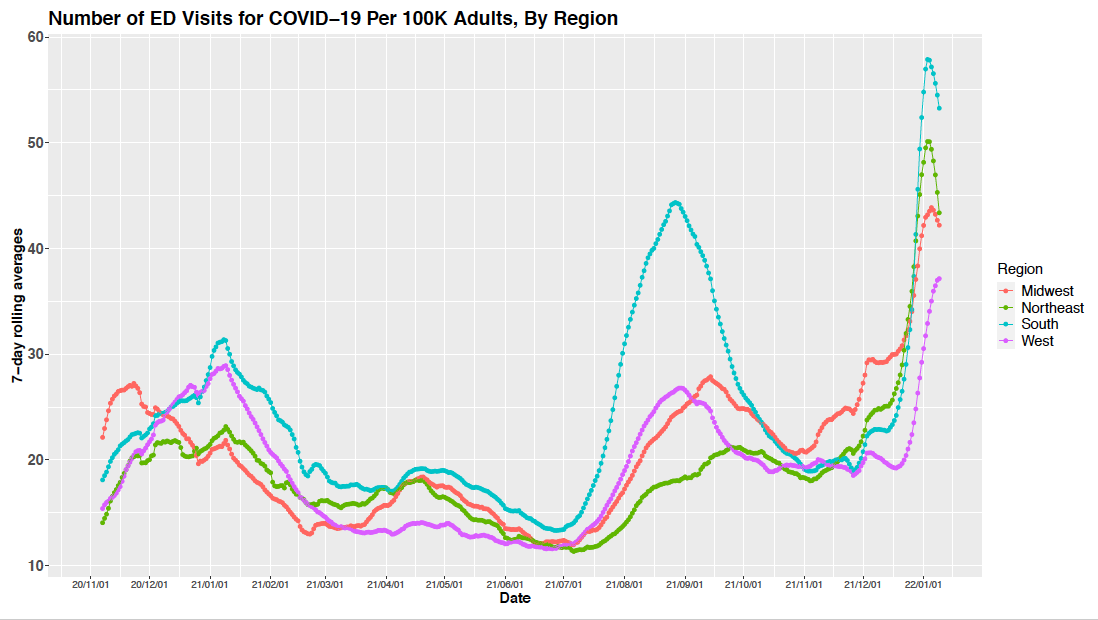
Above is a graph showing the number of emergency department visits for COVID-19 per 100,000 adults by region.
- A review of trends in hospital admissions and census data reveal that the Northeast is likely to lead a national decline in these metrics, with improvements in areas along the northern rim and Pacific Coast likely to be a week or two behind.
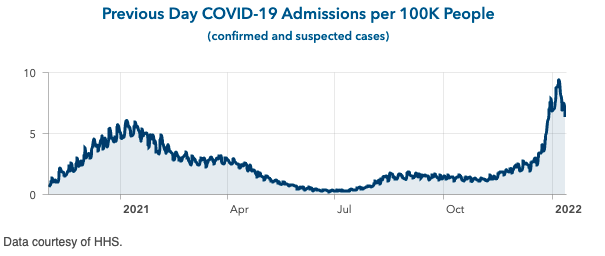
Above is a graph showing previous day COVID-19 admissions per 100,000 people in New York.
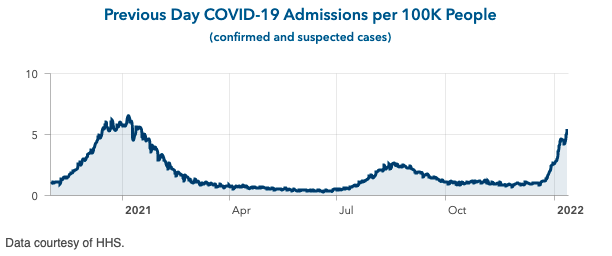
Above is a graph showing previous day COVID-19 admissions per 100,000 people in California.
The nation reaches its peak
Many likely felt anxious this week as national case incidence exceeded 1 million daily cases on January 10, leading to much speculation as to how high both case incidence and hospitalizations may surge as we move further into January. However, our own case incidence projections, emerging trends of declining emergency department visits and hospitalizations, and quickly declining testing positivity data we’re seeing in our region add confidence that much of the I-95 corridor from New York City to Washington D.C., is moving past peaks for both case incidence and hospital admissions.
Through Project: ACE-IT, an in-school testing program in southeastern Pennsylvania that PolicyLab helps administer, we know that testing positivity rates were greater than 20% among asymptomatic individuals who sought testing between Christmas and New Year’s. This week, with nearly 10,000 tests already conducted, the screening positivity rate is back near 2% and falling. While this positivity rate is much higher than what the testing program recorded this fall (0.5% on average), the quick decline is a positive sign that the stress from the current surge may soon recede.
Some may wonder why we are seeing some areas recover when we hit a national record of cases on Monday. The story of this pandemic has always a regional one, and the experience with omicron is no different. Omicron did not arrive to each region simultaneously but instead was introduced at varying time points. As such, the timing of peaks and subsequent recovery will also be highly regional. Furthermore, with many states doing weekly or biweekly reporting, and some no longer reporting on weekends, the batch of test results on Monday, Jan. 10 was likely heavily skewed. This is why it remains important to follow a rolling seven-day average of case incidence that can smooth out this batching phenomenon.
Ultimately, it is clear in this week’s models that population centers in the Northeast and Mid-Atlantic are reaching and moving past peak transmission. More temperate weather in the South may help communities in those states move more quickly past their peaks, even if omicron was slower to arrive there. The Midwest is soon to follow, but we anticipate delays of a week or two for the Pacific Coast as they have yet to reach peak case incidence. Hospitals may recover more slowly, given the higher lengths of stay that adults with severe illness may have, but staffing crises are likely to lessen as the swift spike in case incidence quickly subsides.
Gaining ground for schools
Last week, our team jointly published new COVID-19 school guidance alongside clinical leadership at Children’s Hospital of Philadelphia (CHOP). The guidance aimed to help schools gain some normal footing, even during periods of high community transmission, given the availability of vaccinations to all within K-12 school communities. We prioritize the resumption of in-school education by recommending exposed but asymptomatic individuals can return to school settings wearing a mask. We also recommend less frequent testing of individuals with mild infection or who are exposed but remain asymptomatic in order to simplify school safety plans and overcome limitations in access to adequate, timely testing. The guidance does still recommend that schools continue with masking policies during this period of high omicron case incidence and encourages those who are symptomatic, regardless of testing results, to self-isolate. This combination of recommendations makes in-person schooling feasible, while keeping protective mitigation strategies in place.
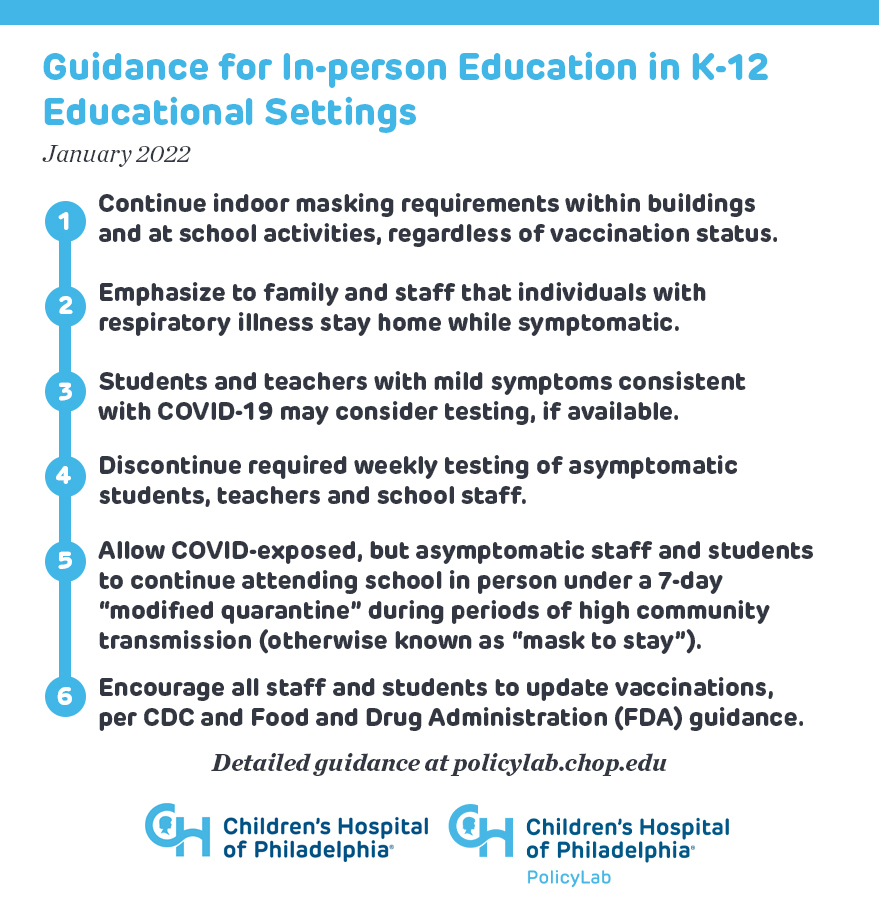
The reception to our guidance has been mostly positive, but we also recognize that some may find it jarring after two years of measures that aimed to eliminate all exposure risk. We need to recognize that we are now at a different stage in this pandemic and a goal of eliminating all exposure risk is not plausible. However, the combination of vaccine availability for all K-12 students and staff, milder illness associated with omicron variant, and a continued commitment to masking policies while in periods of high transmission has made the risk of severe disease from in-school exposure arguably much lower than the risk that many will encounter in their homes or through other community activities. That omicron spread so efficiently while children and teachers were out of school during the holiday break is proof central of this point.
We did receive some specific questions regarding our guidance. Some inquired about how having potentially infectious individuals in school might impact lunches or classrooms with limited ventilation. While we must begin to embrace that no mitigation policy in this moment of widespread transmission can eliminate the presence of infection in our schools, we recognize that lunch might be the highest-risk activity students undertake during the school day. Therefore, we recommend that kids eat outside, when possible, but when that’s not possible, schools should limit mask breaks to only the time it takes to each lunch, maximize ventilation by opening windows, and consider more (and shorter) lunch periods to limit exposure time and create more opportunities for distancing. These should be considered time-limited measures during this period of very high community transmission to minimize student and staff absences. Continued declines in exposure risk may allow many schools to revisit these measures in the next few weeks, but they make practical sense while communities are still at the peak of winter transmission.
We’ve also been asked whether we should be changing the types of masks that children and staff are wearing in schools. We maintain our recommendation for universal mask use in this period of high community transmission, and we prefer 3-ply surgical masks that have been the standard at CHOP since the early days of the pandemic. We are mindful that as case incidence and hospitalizations improve, many schools will move toward mask-optional policies, shifting choices on masking back to families even during periods when the virus is still circulating. We will further discuss mask-optional approaches in our blog posts as we move into periods of lower-case incidence.
Finally, we received lots of questions about staff shortages during this period of high transmission. We understand that schools may have needed to pause in-person learning due to insufficient staff, but we hope our updated guidance, along with the latest Centers for Disease Control and Prevention (CDC) guidance permitting exposed individuals to return to work within 5 days, will help schools navigate beyond this period of uncertainty. The rapidly improving test positivity data recorded through Project: ACE-IT that we mentioned above makes us more confident that by next week, staff challenges are likely to subside in our region and possibly elsewhere.
How soon will schools get back on solid ground?
It became clear to us this week, from regional and national data, that many areas of the country are approaching and moving past peak transmission. Case incidence still remains very high, but test positivity rates in our region are dropping amongst students and staff, suggesting an easier path ahead to normalize school operations and activities. As schools do so, our guidance may help them consider how to begin stripping away measures that were necessary when the goal was eliminating exposure risk, but which are no longer feasible or practical as we must learn to live alongside COVID-19 from here forward.
For now, communities need patience for a few weeks as the crisis begins to abate in our hospitals. We have traveled a long journey to get here. Pivoting on school policy will not be easy for many who have been traumatized by the experience of the last two years, but it will be far easier when it is clear to all that the worst of this crisis has passed. During this period, school staff who are eligible for boosters should obtain them, and families who opted to wait out the first wave of vaccinations for children should quickly reconsider. We anticipate that by February, the country will be rounding a corner, and the arrival of spring soon thereafter will hopefully bring much brighter days.
Jeffrey Gerber, MD, PhD, is associate chief clinical research officer of Children’s Hospital of Philadelphia's Research Institute and co-author of PolicyLab's Guidance for In-person Education in K-12 Educational Settings.
