COVID-19 Outlook: An Especially Challenging Time for Schools
With Labor Day weekend approaching, transmission of SARS-CoV-2 continues to increase in most communities, including among children and adolescents. The resurgence of COVID-19 cases is providing all-too-familiar challenges to returning students to the classroom. Still, school leaders share a common purpose this year: to preserve in-person education, while minimizing absenteeism and the disruptions that COVID-19 has caused over the last 18 months. With that in mind, we provide the September outlook from our COVID-Lab forecasting model for 812 counties across the country. We hope these data coupled with our guidance for in-person education can help school community members, including students, parents, and staff, navigate together their ever-evolving local scenarios as doors reopen and the opening bell rings.*
Here are this week’s national updates:
- The national average PCR test positivity rate is 14.2% this week (up from 13.4% last week). This rate increased since last week in half of the counties we monitor. States with the greatest growth in test positivity include Indiana, North Carolina, North Dakota, Minnesota, Ohio, Pennsylvania, South Dakota and Wisconsin.
- Average case incidence nationwide is nearing 400 weekly cases per 100,000 individuals, with nearly all of the counties we monitor seeing more than 100 weekly cases per 100,000 individuals, a threshold that the Centers for Disease Control and Prevention (CDC) considers “substantial” community transmission.
- Pediatric hospital census grew to 1,400 children over this past week (up from 1,300 last week), before settling back to 1,300 by early this week; the adult census is now just above 100,000 hospitalizations.
- The average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) across the counties we monitor is 1.23 this week; 84% of all counties have a reproduction number above 1, indicating growing transmission. The remaining counties with declining transmission are concentrated in the lower Southeast of the country, which as a region has moved past its peak.
Some regional trends that we are watching:
- Disease activity in the northern half of the country is beginning to surpass that of areas further south.
- As resurgence grows in the north, we are witnessing a within-state trend that we also observed last year: infections increasing first in cities near more rural regions before spreading to larger metropolitan areas. You can see this now in northern Wisconsin and Minnesota, as well as across central Pennsylvania. Notably and expectedly, this is happening in areas with greater numbers of unvaccinated individuals.
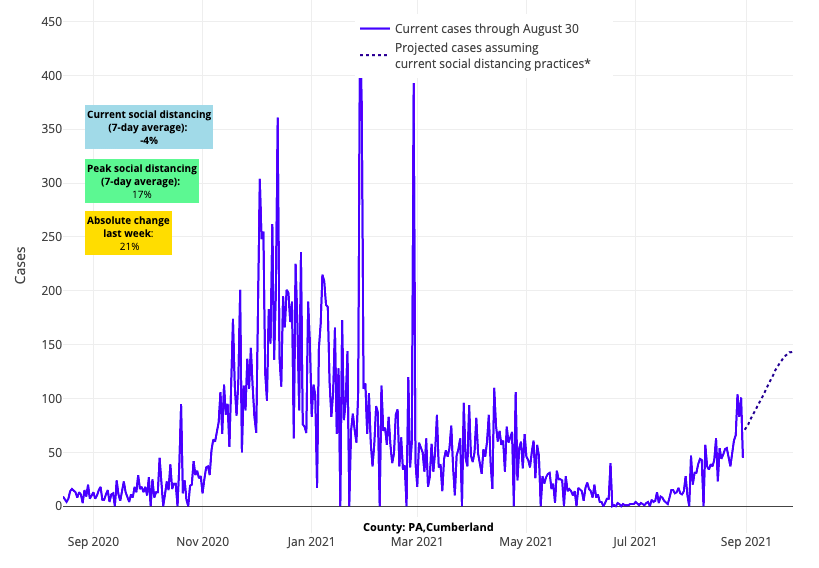
Above are the projections for Cumberland County in Pennsylvania.
- We continue to project substantial growth in case incidence over the next four weeks throughout Indiana. Our models are also forecasting that areas in eastern Ohio are likely to grow quickly in case incidence in the coming weeks, consistent with their low vaccination rates; Pennsylvania may not be far behind.
- The Virginia and Maryland suburbs of Washington, D.C., experienced a modest decline in reproduction numbers and test positivity this week. Despite our models forecasting a continued decrease in reproduction numbers, they will not drop below 1, allowing for the continued increase in case incidence in these areas throughout the month of September.
- Despite some stabilization in case incidence and test positivity rates in the five New York City boroughs this week, we are seeing continued high transmission in the wider metro area, along with growing test positivity extending further south into the Philadelphia area.
- Prior to landfall of Hurricane Ida, our models had forecasted declining transmission in Louisiana. Given the significant displacement of local communities and uncertainty about testing access, our projections for counties in this state are likely to be unreliable for the foreseeable future.
- Out West, our forecasts for counties across Oregon and Washington project a continued increase in case incidence for the next four weeks. Further south, however, the coastal areas of California appear to be stabilizing and reaching summer peaks.
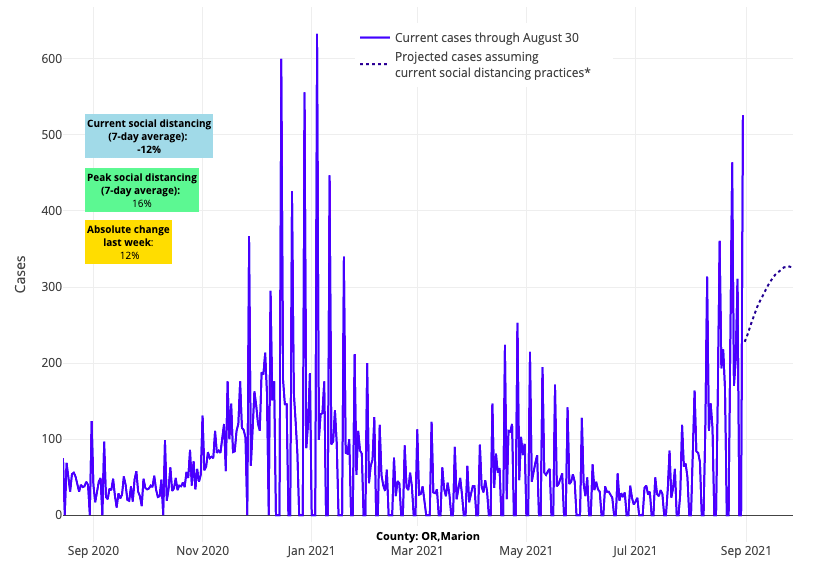
Above are the projections for Marion County in Oregon.
Concern for northern areas grows as progress slows in the south
Similar to our projections from two weeks ago, our models continue to forecast a shift in resurgent transmission from the south to the north. Hospitalizations are quickly increasing throughout northern areas, from the Upper Midwest to the Pacific Northwest and up into Alaska.
With each week of accumulating data, it becomes more apparent that community vaccination rates will dictate case incidence. This week, widespread transmission is evident in Indiana and Ohio—where adult vaccination rates are below 60%—while SARS-CoV-2 transmission and COVID-19-associated hospitalizations are increasing more slowly in states with higher adult vaccination rates like Minnesota (65%) and Wisconsin (68%). However, even if a state has an overall high vaccination rate, local communities with less optimal vaccine uptake are still vulnerable to increased transmission. For example, while overall vaccine uptake in Minnesota and Wisconsin is reasonable, local vaccination rates across their northern-most regions are less robust, and our models forecast more substantial transmission for these regions over the next four weeks.
The Northeast, which has the highest vaccination rates in the country, appears resilient in our models with projected sustained, but slow, growth in case incidence throughout September. This region saw another week with fewer than 75 children hospitalized.
Also notable this week is the slow progress that the South is making. As counties across Arkansas, Florida, Louisiana, Missouri, and Texas slowly move beyond their summer peaks in case incidence, improvements in hospital census are more slowly following. With fall gatherings and school reopenings, we expect to see the current case incidence and hospitalization numbers persist throughout September in this region.
Impacts of School Reopenings are Becoming Clearer
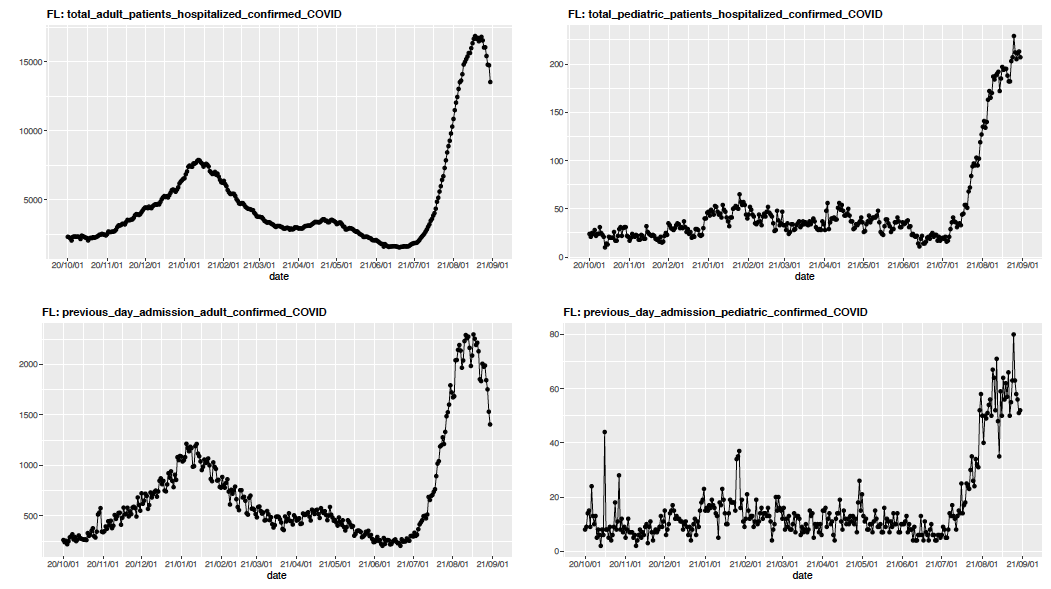
There is now increasing evidence that school reopenings—occurring at a time when children are accounting for a greater proportion of COVID-19 cases—may be delaying progress in areas that were near or moving past their summer peak in case incidence. The experience of some communities where schools have already reopened can provide a cautionary tale for others. For example, even as adult hospitalizations in Florida have slowly moved past peak over the last couple of weeks, there has been a quick rise in pediatric hospitalizations that coincided with school reopenings. Soon after children returned for classes and fall sports, daily COVID-19 hospital census increased from a plateau of 180 children in early August to a new plateau of 225 children that has persisted since the middle of the month.
The above graph (click to enlarge) shows total adult and pediatric COVID-19 hospitalizations and previous day admissions for adults and pediatrics in Florida.
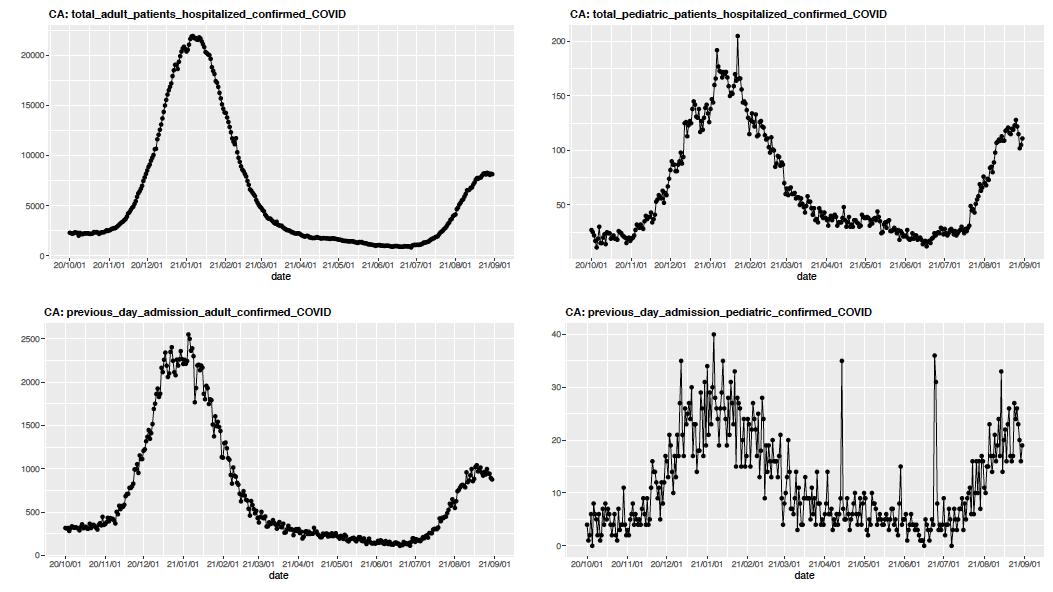
Similar jumps in pediatric hospitalizations can now be seen throughout Georgia and Tennessee. Notably, communities across these states have largely abandoned mask requirements, even as transmission surges. In contrast, California has thus far avoided a similar second bump from school reopenings, illustrating the potential benefit that masking can have when students return to school during a period of substantial transmission. California also benefits from higher community vaccination rates, particularly in its large cities. Our blog post last week illustrated the strong protective effect of adult community vaccination rates on risk for pediatric hospitalizations.
The above graph (click to enlarge) shows total adult and pediatric COVID-19 hospitalizations and previous day admissions for adults and pediatrics in California.
Pediatricians are accustomed to a rise in pediatric respiratory infections within a couple of weeks of schools reopening. As children and adolescents return to the classroom after not seeing peers for several weeks, illness quickly spreads between them. This translates into an influx in primary care office sick visits beginning in the early fall and continuing into the winter. As such, it should not be surprising that a return to school in regions with relatively high transmission rates has led to an increase in COVID-19 infection among children. However, the burden of illness resulting from SARS-CoV-2 spread among students is beyond that of the typical respiratory virus season and has the potential to overwhelm schools ill-equipped to manage the number of infections they might see soon after opening their doors.
For that reason, we believe a requirement for indoor masking at school and throughout a community makes practical sense right now. Our data reveals that nearly all counties in the U.S. are experiencing substantial community SARS-CoV-2 transmission as schools open, and more than 80% are experiencing growing transmission. The priority for all communities this year is to keep children in classrooms, and mass quarantines in the South have already proven extremely disruptive to schools. Masking alongside increased testing and growing vaccinations will help lower COVID-19 burden.
However, the implementation of any required mitigation strategy should be accompanied with an expectation that the need for that strategy be routinely revisited. As community incidence changes, school leaders should be regularly reassessing and adjusting all components of their safety protocols, including mask requirements, returning flexibility in decision-making to families where possible.
While intense debates have emerged at the county, district, and even local school level on how best to manage the year, many communities are recognizing the need to align with public health guidance/requirements. We need to accept that mitigation strategies will need to be fluid throughout the year, dictated primarily by local transmission rates. While the school year is starting out bumpier than people had hoped, schools are better equipped this year to pivot in their safety plans based on their local situations. And if we continue to increase our vaccination rates, we will reduce transmission, ultimately providing our schools more opportunity to roll back mitigation requirements.
As schools return to in-person learning, our team at PolicyLab wishes all students, teachers, and school employees a healthy, safe year. We remain optimistic that even with the challenges of September, there are brighter days ahead.
*Frequent visitors to the COVID-Lab model will note some adjustments to our projections, which now incorporate a rolling seven-day case incidence (as opposed to daily rates) to account for increased noise in the data and unreliable daily reporting in many regions. This change has improved the validation of our model over prior weeks, and our projections for reproduction numbers and case incidence for the next four weeks appear smoother than in previous forecasts. We’ve also decided not to include projections for counties across Nebraska, as concerns about reliability of data have arisen over the summer.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia and co-author of PolicyLab's Guidance for In-person Education in K-12 Educational Settings.