COVID-19 Outlook: As Recovery Continues, Schools Plan for Next Steps

A review of our COVID-Lab forecasting model this week reveals COVID-19 transmission and hospitalizations are declining across most of the U.S., and those regions slowest to improve are likely to move past peak case incidence and hospital census over the first or second week of February. Our weekly blog post reviews those data and discusses how the improving situation may influence school safety plans at this stage of the pandemic.
First, let’s review hospitalization trends and projections:
- National adult hospital census is around 120,000 patients, a 25% decrease from its peak just a couple of weeks ago. Pediatric hospital census is at 3,500 patients, a 30% decrease from two weeks ago. During the same period, adult and pediatric hospital admissions dropped by nearly 50%.
- States that experienced the highest adult hospital census (70+ patients per 100,000 residents) over the last week include West Virginia, Alabama, Nevada, Arkansas, Missouri, Mississippi, Oklahoma and Kentucky. States with the largest proportional increases in pediatric hospitalizations are along the northern rim of the country and in the Heartland.
- Despite a difficult last few weeks, Arizona and New Mexico are seeing sharp declines in emergency department visits, and our projections show they will soon see substantial declines in hospital census as they move past peak admissions. A similar trend is occurring across the Heartland.
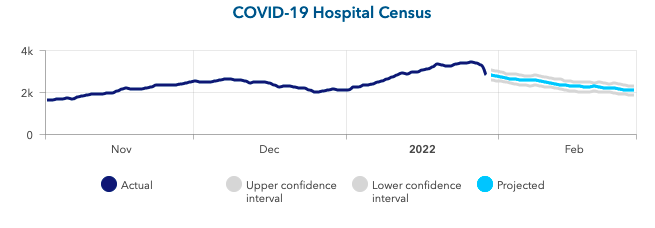
Above is a graph showing COVID-19 hospital census (actual & projected) in Arizona.
- Our models now suggest the grip of the current resurgence along the northern rim of the country is beginning to abate, as we project hospitalizations and case incidence in these states will decline more quickly over the next four weeks than in areas in the Mountain West and Pacific Northwest.
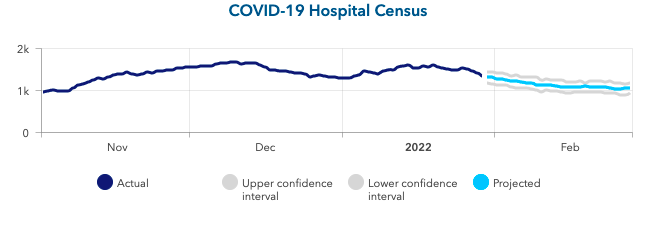
Above is a graph showing COVID-19 hospital census (actual & projected) in Minnesota.
- Parts of the Southeast (Kentucky, Tennessee, West Virginia, North Carolina, Alabama and Arkansas) have experienced a surprisingly slow recovery this winter. Our models for these states and current trends in emergency department visits suggest a pace of improvement similar to the Pacific Northwest, which is expected to move past peak in the next 1-2 weeks.
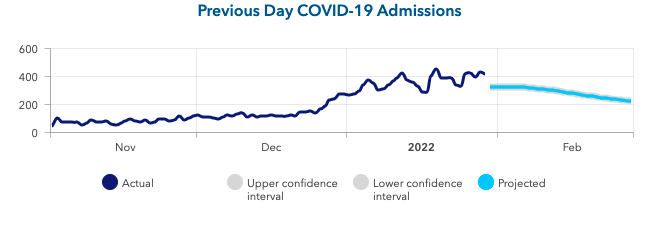
Above is a graph showing previous day COVID-19 admissions (actual & projected) in Tennessee.
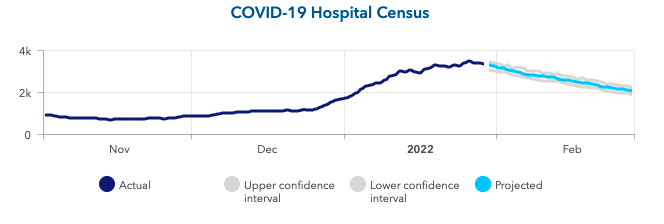
Above is a graph showing COVID-19 hospital census (actual & projected) in Tennessee.
Other national and county-level trends we are seeing:
- The average national PCR test positivity rate across the 812 counties we follow in our models declined to 28.7% this week, down from 33% last week. Testing positivity is declining in all states except Wyoming and Tennessee.
- The average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) is now 0.79, with 85% of counties below 1, indicating declining transmission (up from 40% of counties last week).
- Average county-level case incidence declined to 1,200 weekly cases per 100,000 residents from nearly 1,500 weekly cases per 100,000 residents last week. All counties are still above 200 weekly cases per 100,000 residents.
- Within metropolitan areas experiencing sustained transmission, case incidence remains higher (and often increasing) in collar counties, even as cities are improving. This can be seen in places like Dallas, Houston, San Antonio, Nashville, and Seattle, which are now all improving, but the counties surrounding these cities have higher reported case incidence than within the cities themselves.
Taken together, these data and our projections show that most areas of the country are actively improving and areas seeing sustained impacts will join these regions in the next couple of weeks.
What do widespread improvements mean for schools?
As case incidence quickly falls across most of the country, and as hospitalizations begin to follow, our team has received many questions over the past two weeks about when schools might transition to mask-optional policies for both students and teachers.
From our perspective, decisions regarding mask mitigation strategies cannot be solely based on whether or not masks are effective at reducing transmission—they are effective. However, other factors—such as community case incidence, the risk of severe disease following infection and the competing risk of maintaining strict requirements—must be considered in the decision-making process. These remain inherently very local decisions, pursuant to knowledge of local public health codes and orders and the needs of individual communities. When deciding between mask-required versus mask-optional strategies, the overarching question is whether the same level of required safety measures is still necessary. For example, mask use will have more benefit when case incidence is high and be less effective when case incidence—and by extension, exposure risk—is low. Therefore, communities experiencing a decline in case incidence may now have an opportunity to weigh the benefits of continuing with strict adherence to certain school mitigation requirements against the competing risk that these mitigation strategies may inhibit the normal operations of a school day.
We acknowledge that a transition away from mitigation requirements, such as moving from mask mandates to mask-optional policies, may lead to anxiety across some school communities. In that context, we offer perspective as to when and how schools might consider making this transition and how families might navigate their own choices in response.
First, we continue to support mask requirements in schools located in counties yet to experience a significant reduction in their case incidence and hospitalization burden. Some regions are still at their peak case incidence, necessitating patience to allow hospitals to respond to this crisis, particularly with many hospital and school staff still out for illness or to care for household members. Second, we urge school leaders to defer to public health code and continue seeking guidance from local health departments. If mask mandates are still in place by public order for schools and other community settings (as they are in many large cities), we would expect that schools would honor them as part of a collective response within these regions.
Next, we must ensure that community members are provided an accurate assessment of risk of infection for themselves and their families. The arrival of omicron resulted in widespread transmission across a substantial proportion of the population since early December. While omicron can still cause severe illness, especially in those who are unvaccinated, it has been associated with milder symptoms for most individuals. After recent widespread transmission of omicron, many communities have experienced a decline in case incidence during the last few weeks. As case incidence declines, so too does the risk for transmission.
In our own community, weekly testing of all school staff, which has continued in the School District of Philadelphia as part of their safety protocols, has revealed that rates for asymptomatic infections have quickly dropped to 1 in 200 individuals, from 1 in 4 the week after Christmas. And as case incidence has dropped abruptly, regional adult hospital census has also dropped by half, and pediatric hospital census by nearly 80% in the last couple of weeks. While our weekly asymptomatic screening rate is still higher than the pandemic low of 1 in 1,000, its abrupt decline suggests that exposure risk may near those low levels by the end of February.
Finally, for schools based in areas where health departments no longer require indoor masking or whose leaders are planning to make this transition in the coming weeks, we emphasize the value in continuing to equip families with the most current recommendations and information from local health authorities and the CDC. If health departments still recommend but do not require indoor masking at current case incidence rates, it is likely that many families and children will continue to mask, even if others elect a different choice. In the school guidance we provided in August 2021, we provided a chart to help families navigate their own decisions around masking once schools shifted to mask-optional policies. We emphasized then, as we continue to do now, that the risk of exposure in schools would highly depend on community case incidence; as case incidence fell, so would the risk of transmission at school. We further noted the importance of considering vaccination status of the individual and vaccine rates of the school and greater community, as well as consideration of specific risk factors such as underlying comorbidities for the individual or other household members.
Ultimately, school COVID-19 policies at this moment should prioritize access to in-person education for all and incorporate mitigation approaches that mirror the current state of the pandemic. In doing so, schools will recognize moments when more flexible policies are possible and can permit choices for families, who themselves are weighing their own concerns about the risk of infection from this virus against the competing risks to their children and from other challenges in their lives.
Jeffrey Gerber, MD, PhD, is associate chief clinical research officer of Children’s Hospital of Philadelphia's Research Institute and co-author of PolicyLab's Guidance for In-person Education in K-12 Educational Settings.
