COVID-19 Outlook: Forging Forward from the Pandemic

Now that spring break and the Easter and Passover holidays have passed, our COVID-Lab team returns this week to review regional and state emergency department visit and hospital admission trends. In many regions, particularly in the Northeast, there have been relatively modest increases in emergency department visits and hospital admissions during the past few weeks, creating uncertainty for the weeks and months ahead. We aim to provide context for these trends and offer our projections for what is to come.
Here's what this week’s data reveal:
- National COVID-19 hospital census for patients with confirmed infection fell last week by 5% and was below 10,000 patients at the start of the week. This milestone represents a more than 90% decline from a peak of nearly 150,000 individuals in early January 2022.
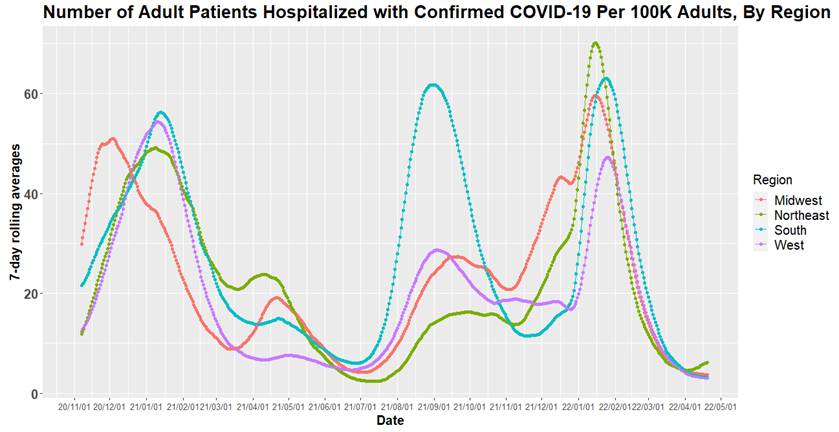
Above is a graph (click to enlarge) showing the number of adult patients hospitalized with confirmed COVID-19 per 100,000 adults, by region.
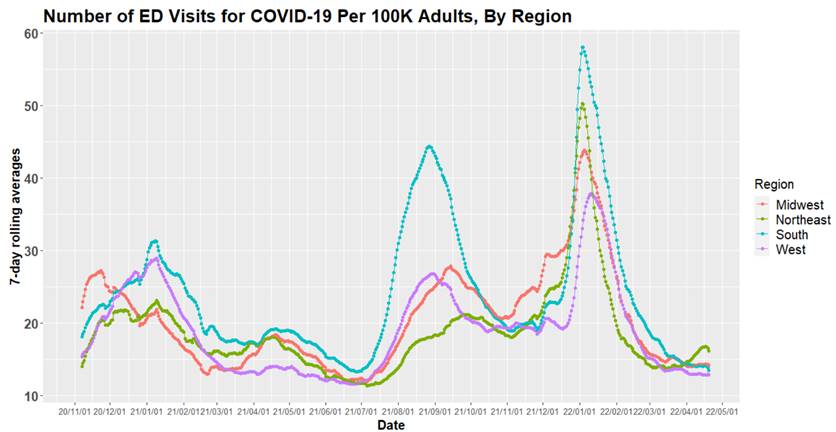
Above is a graph (click to enlarge) showing the number of emergency department visits for COVID-19 per 100,000 adults, by region.
- Some Northeastern states, such as Massachusetts and Connecticut, experienced a more than 10% increase in hospital census for patients with confirmed COVID-19 infection last week. Even with these increases, only two states, New York and Vermont, had more than 5 COVID-related hospitalizations per 100,000 individuals. This week’s data suggest that this uptick will be brief as adult emergency department visits and hospital census have begun declining across the Northeast.
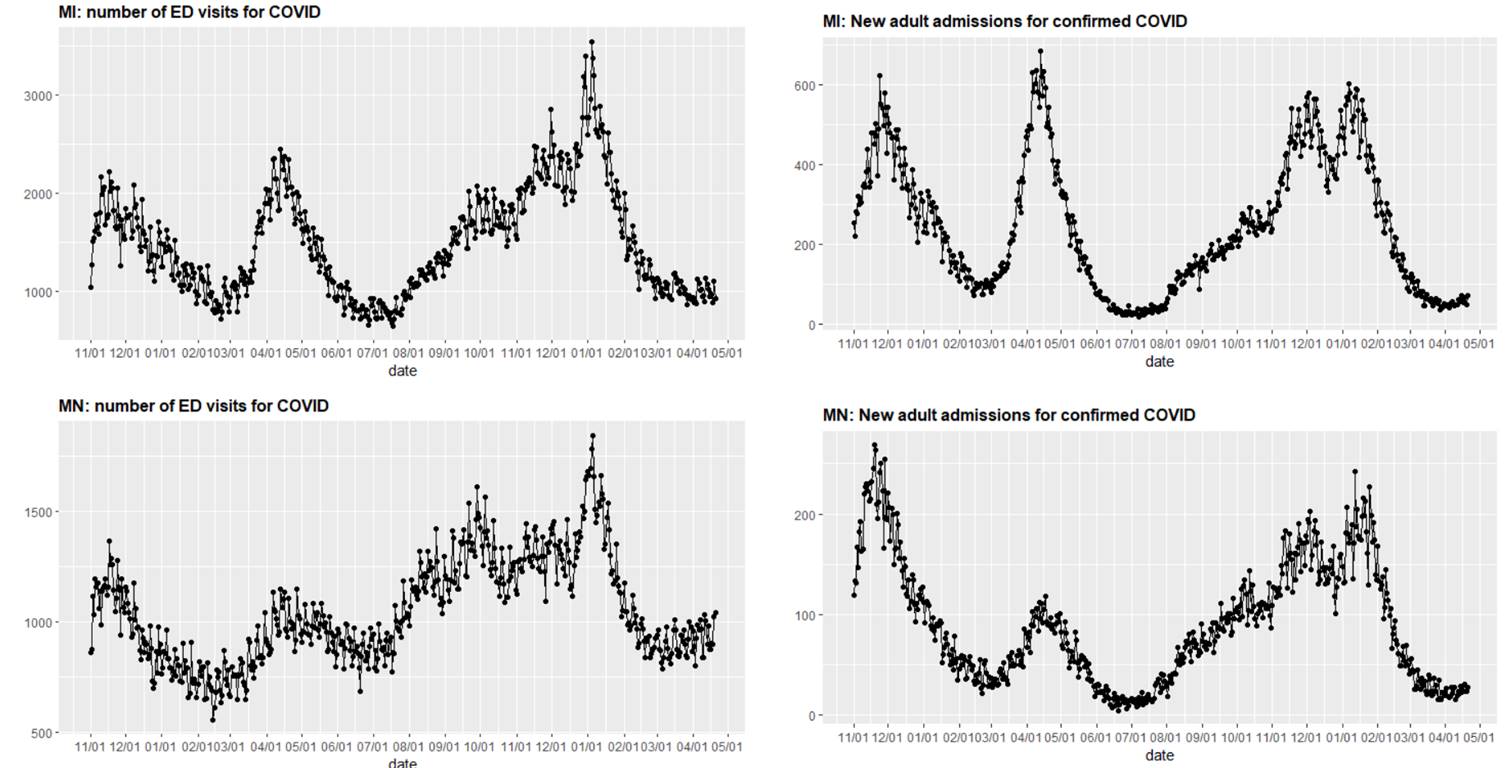
- The Upper Midwest has experienced only slight increases in emergency department visits compared to prior waves, including during a similar time period last spring. Hospital census in this region remains flat.
Above are graphs (click to enlarge) showing the number of emergency department visits for COVID-19 and new adult admissions for confirmed COVID-19 in Michigan and Minnesota.
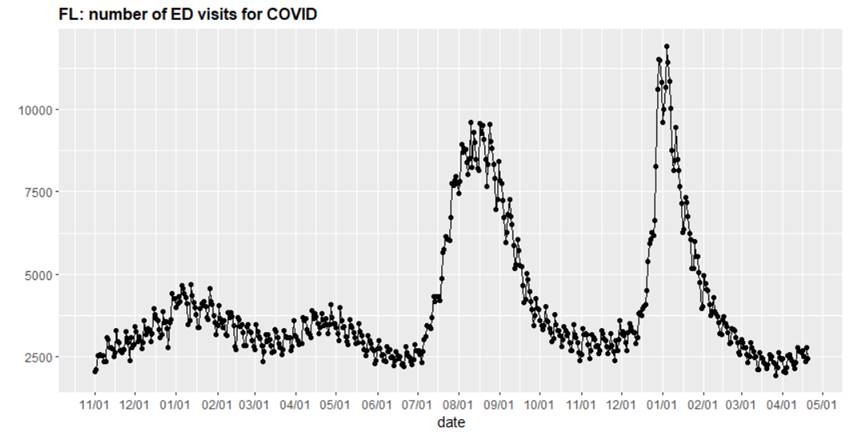
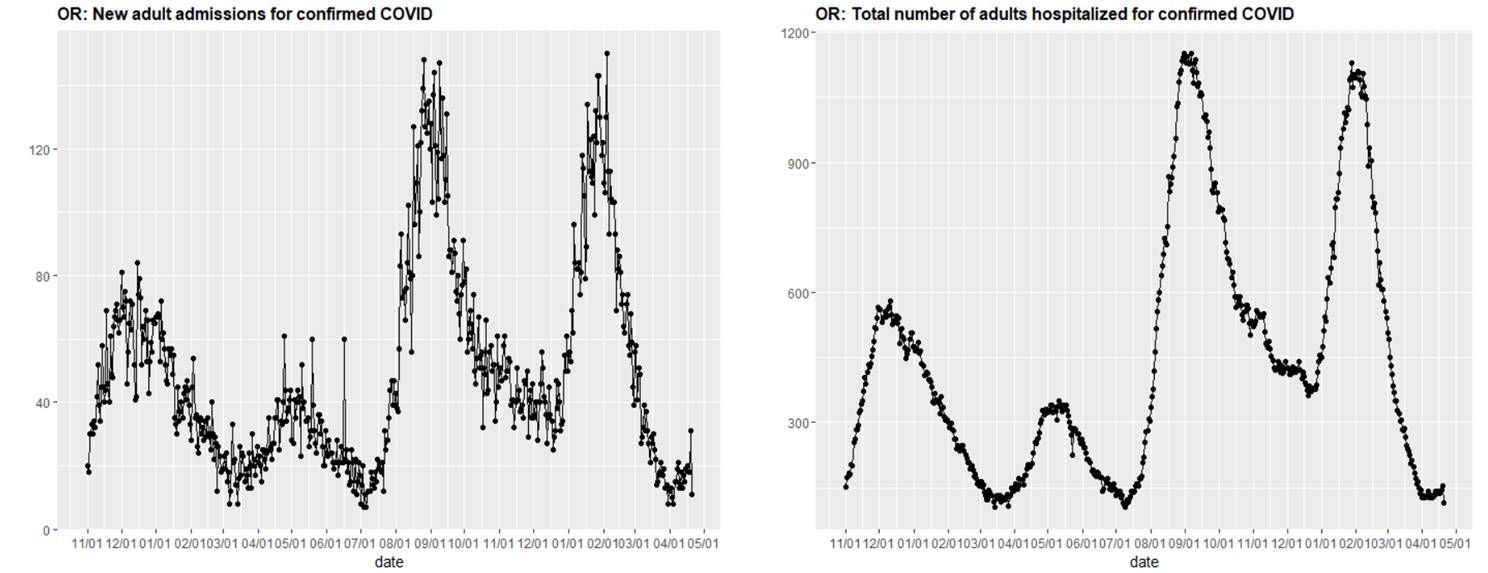
- The lower Southeast is experiencing an increase in emergency department visits following the spring holidays. New COVID-related admissions have slightly increased in some states in the Pacific Northwest, namely Idaho and Oregon, but overall hospital census has remained stable in this region. Both the Southeast and Pacific Northwest bear closer monitoring in the coming weeks.
Above is a graph (click to enlarge) showing the number of emergency department visits for COVID-19 in Florida.
Above are two graphs (click to enlarge) showing new adult admissions for confirmed COVID-19 and the total number of adults hospitalized for confirmed COVID-19 in Oregon.
- The Southwest continues to remain stable with declining hospital census across a wide region.
Interpreting Current Trends in the Context of the Last Two Years
Recent upticks in cases, emergency department visits, and hospitalizations have led to unease amongst some families and public health officials, triggering concerns that another substantial resurgence of COVID-19 is right around the bend. However, we have guarded optimism as we move further into spring, given the fairly modest impacts that the lifting of mask requirements and increase in travel and family gatherings for spring breaks and holidays seem to have caused. We suspect that these changes may have led to the recent modest increases in transmission but note that they are already subsiding in many areas.
Our confidence in this assessment is further supported by our experience in school-based COVID-19 testing through Project: ACE-IT. This week, we have seen a declining rate of COVID-19 positivity among asymptomatic School District of Philadelphia staff who are participating in ongoing surveillance testing. During the week of April 3, 1 in 133 tested staff members had detectable virus; early this week that had fallen to 1 in 250.
In contrast to the large wave of hospitalizations this winter triggered by the omicron variant, the current increase can more aptly be described as a ripple. Further, the declining trends beginning in the Northeast, and the relative resilience of areas south and west, suggest that we are unlikely to see substantial growth in hospitalizations and that there will be continued improvements for many locations in the coming weeks.
One area that does bear watching is the Southeast where, for example, Florida emergency department visits are increasing. In past years, spring travel to the Southeast appeared to trigger the beginning of prolonged summer waves. We are hopeful that the relatively modest impacts experienced thus far in other areas of the country will be realized in the Southeast as well, but time will tell.
Taking stock of what we have learned and pivoting
Throughout the last two years, our team has recognized that COVID-19 guidance needs to be adapted and updated to align with the current state of the pandemic, which has now transitioned away from a national public health emergency. Early in the pandemic, our primary defense against COVID-19 was to limit person-to-person transmission via social distancing and mask use. These strategies were necessary to buy time and save lives until more sustainable interventions, such as vaccinations and improved treatment strategies, were available. In those early stages, our team homed in on community case incidence as our best measure of pandemic risk. These data and our modeling projections allowed us to anticipate the winter wave of 2020-21 for what it became: the height of a national public health emergency and a period when half of all American fatalities occurred.
Fortunately, in 2021, testing became more widely available and effective vaccines were offered to all adults. Now well over a year into vaccine availability and outreach, population immunity from vaccination coupled with immunity from natural infection is great enough that we believe fewer population-wide public health measures are needed. Yes, it is true that many of us have family members, friends and colleagues who are now becoming infected. But it is also true that they, on average, are not experiencing serious disease and are not requiring hospitalization. These observations and the relatively modest impacts on hospitalizations during this spring resurgence suggest that today’s COVID-19 cases are less severe than what we experienced in 2020 and 2021 and, therefore, the mitigation measures we take today can also be less stringent.
We are not the only epidemiological group making this assessment. Other epidemiology teams, including those at the Centers for Disease Control and Prevention (CDC), are also now following hospitalization trends and linking community recommendations to these measures. As we note above, hospitalizations have remained relatively low and are now declining in most areas. This fact should instill confidence that we can continue thoughtful reductions in our restrictions and avoid reinstating requirements unless hospitalizations begin to rise significantly. Simultaneously, we should continue to focus on optimizing resources that bolster vaccination rates and improve awareness of newly available effective treatments across all communities.
This is not to say, however, that there are no more uncertainties with this pandemic. These last two years have taught us to be aware that things can change, necessitating our mitigation measures to change. We will continue to monitor closely for evidence of worrisome trends in the epidemiology of hospitalizations related to COVID-19. Researchers will continue to work to optimize vaccines, provide data to inform vaccine boosting schedules and bring novel therapies to market. Make no mistake, SARS-CoV-2, the virus that causes COVID-19, will continue to exist. But continuation of mandatory population-level mitigation strategies, such as mask mandates, will not eliminate this virus, which is destined to become endemic with impacts more comparable to other seasonal respiratory viruses.
What families and school leaders are asking us now
As the COVID-Lab team begins to deconstruct the scaffolding of our own two-year journey with this pandemic, we return once again to questions from families and school leaders that have served as our North Star from the first day we began collecting and interpreting data related to the COVID-19 pandemic. Analyzing local area data to help families and school leaders navigate through a generational crisis was our mission from the get-go, and our dialogue with these individuals has been the most rewarding part of our COVID-Lab journey.
In that spirit, today’s most frequently asked question is how communities should host traditional year-end events for youth such as prom and graduation. Our response has been: “have prom, have graduation.” It is still reasonable and logical for school communities to seek outdoor or larger venues to allow people space to congregate—leveraging opportunities for outdoor ventilation and limiting indoor overcrowding is beneficial to reducing the transmission of any respiratory virus.
Yes, it is possible that transmission of SARS-CoV-2 or other viruses will take place at these events. Should clustered outbreaks occur, communities can be notified and testing can be offered. However, we have come a long way from the start of this pandemic and our children have sacrificed many opportunities for learning and experiencing important life milestones. The potential for clustered outbreaks should no longer be a deterrent for hosting these events. It’s important that our children and families get back to the experience of normal, and we must redouble our efforts to catching kids up in school and promoting the resilience and well-being of our school communities as they emerge from the pandemic.
Given the overall improvement nationally and the resilience against substantial surges in hospitalizations that is evident in our regional and national data, our team intends to significantly reduce the cadence of our COVID-Lab reports. We will still continue to monitor regional trends in the weeks and months ahead, but we will no longer post regular updates to our website, taking down our data dashboards and choosing instead to link through our PolicyLab project page to the terrific CDC data site that regularly provides regional updates on many metrics, most notably hospitalizations and genomic variation of emerging COVID-19 strains. If we see significant changes that warrant discussion, we will use PolicyLab’s Twitter account to connect with our readers. We will also return from time to time, should conditions warrant, to discuss findings in further detail through our blog and answer emerging questions from families and school communities.
Jeffrey Gerber, MD, PhD, is associate chief clinical research officer of Children’s Hospital of Philadelphia's Research Institute and co-author of PolicyLab's Guidance for In-person Education in K-12 Educational Settings.