COVID-19 Outlook: Tackling Unresolved Questions about Children as Recovery Continues

We return this week after a brief hiatus from providing COVID-Lab modeling updates to offer our latest outlook on the state of the pandemic. Our team is no longer producing county-level case incidence projections, as case incidence data have become less reliable around the country. However, we continue to monitor hospital census and emergency department visits across the states. Even in the absence of projections, these metrics can serve as important indicators for how much COVID-19 is impacting communities. Currently, some countries in Europe are experiencing another increase in hospitalizations and emergency room visits that has been attributed to the evolution of the omicron variant. Continued assessment of these metrics locally will be important to detect any signal of potential resurgence in the U.S.
Here are this week’s updates on hospital census and emergency room visits:
- National adult hospital census declined below 20,000 individuals this week, down from 30,000 just 10 days ago and down from 150,000 in early January 2022. National daily adult admissions have dropped below 1,500 patients per day for the first time since last June. Only Vermont and Montana are showing a higher number of adult admissions this week than last.
- Pediatric hospital census declined this week to 600 children, down from 950 just 10 days ago. No states documented an increase in pediatric admissions this week. This pediatric census is still far above last spring and similar to late fall, suggesting that the decline in pediatric hospital census has been slower than for adult hospital census over the last few weeks.
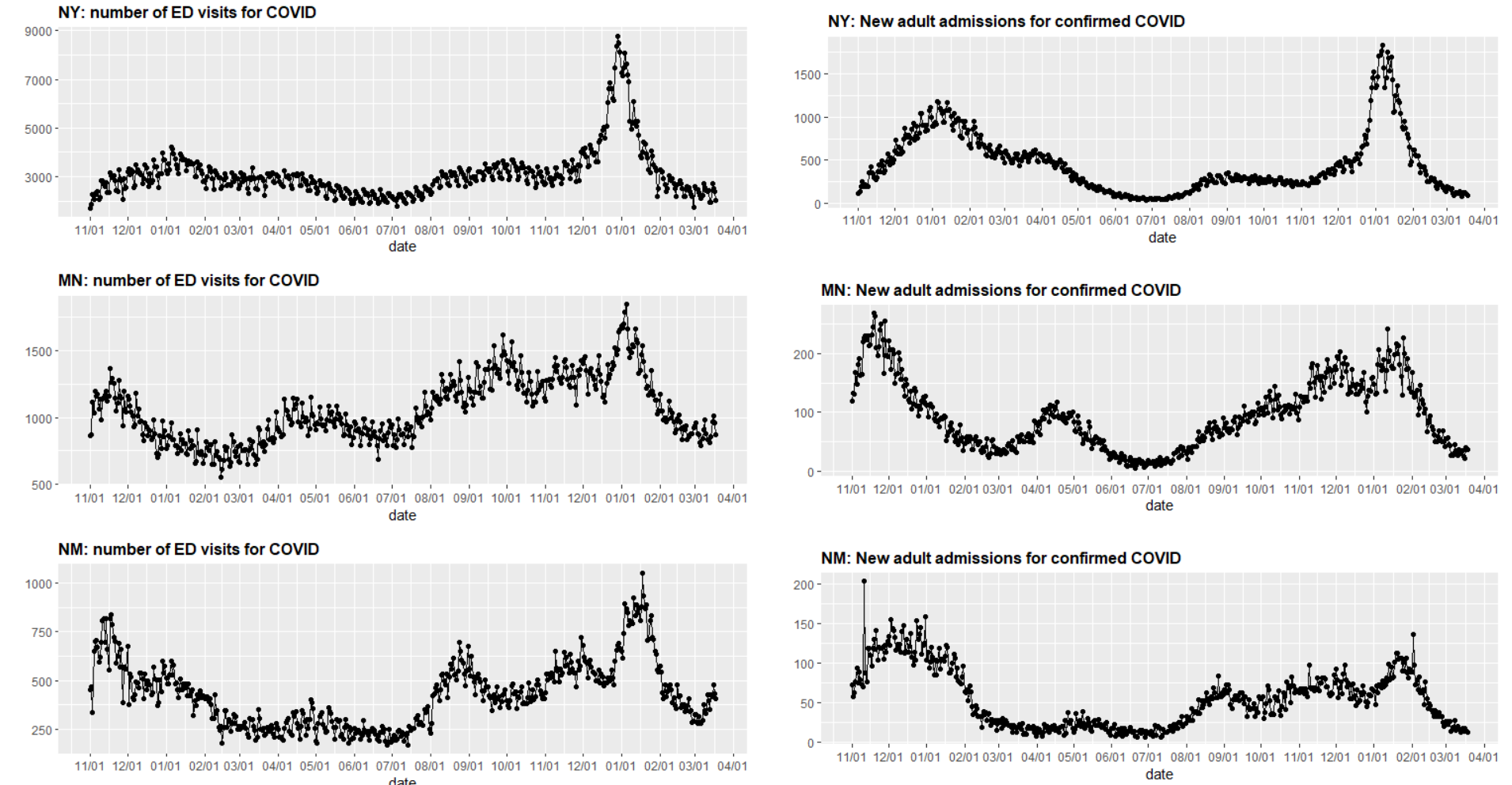
- Eighteen states have stable or slightly increasing emergency department visits. This includes multiple states in the Northeast, Upper Midwest and Mountain West. Even as emergency department visits have increased in some states like New York, Minnesota, and New Mexico, thus far they have not been accompanied by a significant increase in hospital admissions.
Above are multiple graphs (click to enlarge) showing the number of COVID-19 emergency department visits and new adult admissions for confirmed COVID-19 cases in New York, Minnesota and New Mexico.
- Some states have already experienced short-lived increases in emergency department visits. For example, Georgia saw emergency department visits increase in mid-February but has seen improvements in the last two weeks.
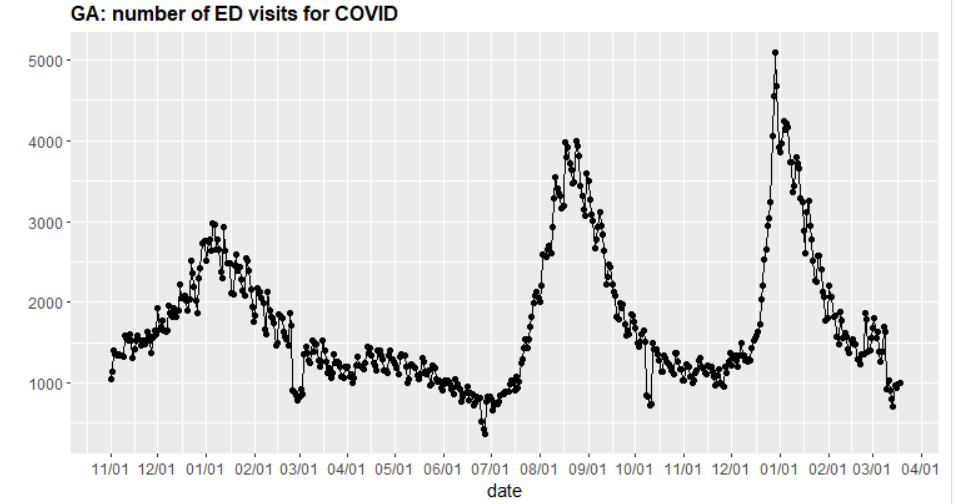
Above is a graph showing the number of COVID-19 emergency department visits in Georgia.
COVID-19 Infections Remain Low Across Most Regions
With the nation experiencing a broad, swift recovery following the winter omicron wave, the Centers for Disease Control and Prevention (CDC) removed recommendations for continued adherence to indoor masking. This has led most settings to transition to mask-optional policies and has increased social interactions. While this return to some normalcy is welcomed by many, increasing cases in Europe from a subvariant of omicron BA.2 does instill some concern about what might await us in the coming weeks.
Based on our review of the current data, we think it is premature to suggest that another impactful wave of transmission will emerge across the country early this spring. Certainly, with more places being mask-optional, it is likely that we will see some increases in transmission. Areas with residual disease burden—particularly colder regions or places that have yet to experience high rates of infections among residents—may see a rise in case incidence that exceeds other communities where immunity from natural infection or vaccination is higher. Increasing travel with spring break might also exacerbate these trends. This is already evident in some states in the Northeast, Upper Midwest, and Mountain West where emergency department visits are either no longer declining or starting to increase slightly.
While these trends in emergency department visits do raise concerns for what may come, there are factors that could limit the magnitude of a resurgence at this time. Warmer weather has moved into most regions, which should allow people to spend more time outdoors where transmission is less efficient. Additionally, the omicron wave and continued vaccination efforts have reduced the number of individuals susceptible to COVID-19. These factors may blunt a substantial surge posed by the increasingly prevalent omicron BA.2 subvariant. To this point, we are particularly interested in the trends from Georgia over the last four weeks. In mid-February, residual omicron transmission trended higher across the state with a significant increase in emergency department visits, but very quickly by early March, resumed its downward trajectory, much like most areas of the Southeast.
We may yet again have arrived at an inflection point. As masks come off and social interactions increase, it is certain that there will be some rebound in transmission. But thus far, continued declines in hospitalization have suggested that this inflection point may not be substantial nor prolonged. We will need to monitor emergency department visits and, more importantly, hospitalizations to understand the impacts of this in the coming weeks. Hopefully, the experience in Georgia will play out in other locations and hospitalizations will remain low and continue declining. Either way, our team will be monitoring trends in both emergency department visits and hospitalizations and will report any concerning shifts we identify in these metrics.
Making sense of vaccination data in younger children
Over the next couple of weeks, Moderna and Pfizer are likely to submit data to the Food and Drug Administration (FDA) on vaccine effectiveness and safety for their COVID-19 vaccines in children between 6 months and 5 years of age. These submissions are coming at a time when analyses that question the duration of vaccine effectiveness against infection or hospitalization in older pediatric patients are being released to the public (prior to completing the peer review process). The availability of such results, especially as the CDC and FDA debate vaccine effectiveness in our youngest children, may be confusing to many parents. These data—coupled with declining rates of COVID-19 infection and the notion that illness in children is often less severe—may also reduce the urgency of some parents to pursue vaccination for their children.
We would like to provide three important points of context for this important decision as we are confident that vaccinating children remains an important step for their protection as well as the community around them:
1) Data on waning immunity to vaccinations, particularly in children, understate the value of vaccination in protecting children from severe COVID-19 infection. During an omicron wave in which so many children were infected in such a short period (for example, Project: ACE-IT testing in Philadelphia estimated that 25% or more of youth were infected with COVID-19 at the end of December), the spectrum of illness varied. Some children were asymptomatic, some had symptoms of the common cold, some developed croup or asthma exacerbations requiring brief hospitalization, and finally, although rare, some children had severe COVID-19 symptoms requiring intensive care. Importantly, the vast majority of children requiring intensive care for COVID-19 were unvaccinated. This is not a trivial point; the goal of the vaccine is to prevent severe infections, and not vaccinating a child is a missed opportunity to prevent severe disease.
2) While severe outcomes from COVID-19 are less common in children, they have been more frequent than other common pediatric infections that we routinely care for each year. CDC estimates that 1,341 children have died in the U.S. during this pandemic. Although only 0.1% of all U.S. COVID-19 deaths, this is higher than the typical number of child deaths from influenza that we see in a two-year period. The continued benefit of vaccination against severe disease is the principal reason our teams at Children’s Hospital of Philadelphia (CHOP) continue to urge all children to get vaccinated against COVID-19 as soon as the vaccine is deemed safe and efficacious for their age group.
3) Children can serve as a source of transmission to vulnerable adults. Even with a milder variant, widespread transmission still resulted in more than 200,000 individuals succumbing to COVID-19 infection this winter. Vaccination of people of all ages, including children, can reduce chains of transmission so fewer adults are hospitalized or die. As we anticipate future resurgence of COVID-19, particularly next winter, families should consider vaccinating children as part of a collective response to shield older family members and neighbors from disease or death.
What’s next for the vaccine approval process?
Although frustrating for parents, the vaccine approval process is seeking to find the safest dose and interval of vaccine doses to minimize safety concerns while maximizing protection against severe infection. This spring will see the FDA consider data for kids under 5 years of age who are awaiting their opportunity. These data will include results from Pfizer’s three-dose vaccine for 2-4-year-old children and Moderna’s two-dose vaccine for 2-5-year-old children; both companies are also assessing similar doses and schedules for children ages 6 months to 2 years. It is unclear if data for this youngest subgroup will be presented to the FDA along with the data for 2-5-year-old children or be submitted later.
What to do about children under 5 years of age
Until the FDA issues an emergency use authorization for COVID-19 vaccines for children under 5 years of age, public health experts and early childhood education staff will continue to debate the necessity of mitigation measures, particularly masking of children and staff. In January, when CHOP and PolicyLab released our COVID-19 guidance for children in early care and education settings, our team anticipated that once the winter surge receded, the only settings in which mandatory masking might continue would be early childhood education and health care. With the risk of severe disease lowest in the youngest children, we recommended that early childhood settings pivot to optional masking when their local K-12 partners did. We continue to recommend this; at this point of the pandemic, an enhanced level of population immunity coupled with a less virulent virus makes this approach even safer. It is time to permit families flexibility in early childhood settings, and we would strongly encourage those settings that have delayed a transition to mask-optional policies to make the change.
Our team intends to continue following weekly trends of emergency department visits and hospitalizations and will return with another analysis should substantial resurgence occur.
Jeffrey Gerber, MD, PhD, is associate chief clinical research officer of Children’s Hospital of Philadelphia's Research Institute and co-author of PolicyLab's Guidance for In-person Education in K-12 Educational Settings.