COVID-19 Outlook: Preparing to Vaccinate Children as Our Nation Reaches a Turning Point

Below are the main findings from the weekly update to our COVID-Lab forecasting model:
- The national PCR testing positivity rate remains unchanged between this week and last week at 6.3%; however, fewer of the 821 counties we follow in our model saw increasing test positivity rates (43% vs. 50%).
- The national average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) dropped from 1.16 last week to 1.09 this week. The proportion of counties we follow with reproduction numbers over 1.25 dropped from above 20% last week to 16.5% this week.
- Daily COVID-19-related hospitalizations have started to recede, with just under 40,000 adults and 1,000 children hospitalized nationally.
Summary of data by region:
- Communities across the Midwest are seeing declining PCR positivity rates and reproduction numbers, including in Minnesota, Illinois, Michigan, Indiana and Ohio. In Illinois, improvements in test positivity and case transmission in multiple counties surrounding Chicago suggest that area is moving past its current peak; our forecasts show declining case incidence over the next four weeks.
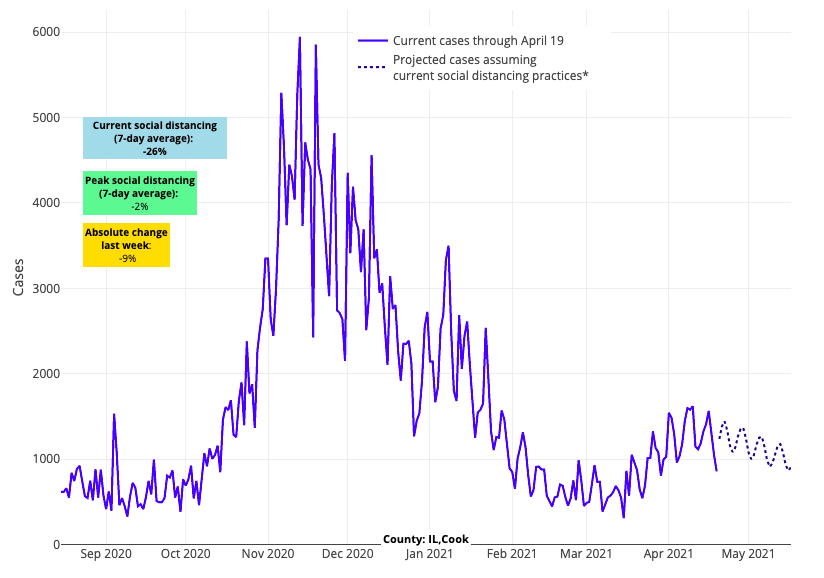
Above are the projections for Cook County (Chicago) in Illinois.
- Reproduction numbers are now below 1 in all five New York City boroughs and throughout the surrounding metropolitan area. Our models project continued declines in case incidence for this region in the coming weeks.
- Many areas in the Northeast and Mid-Atlantic improved this past week. These improvements have been slowest in southeastern Pennsylvania and Delaware, where higher rates of positivity and hospitalizations persist. However, our models forecast that this region will experience declining case incidence in the coming weeks.
- The data from Florida this week are the most difficult to interpret. Testing positivity rates and reproduction numbers appear to be increasing in some counties but decreasing in others. This suggests that some counties may see flat but high case incidence in the coming weeks, while others may experience growing case incidence. There has been a 25-30% growth in hospitalizations across Florida recently. This bears watching, but these hospitalization numbers are still well below winter peaks and mortality is still low.
- Colorado, particularly Denver and Colorado Springs, had been experiencing increases in testing positivity rates and reproduction numbers in recent weeks, but these metrics have improved, and our models forecast continued declines in case incidence for the weeks to come.
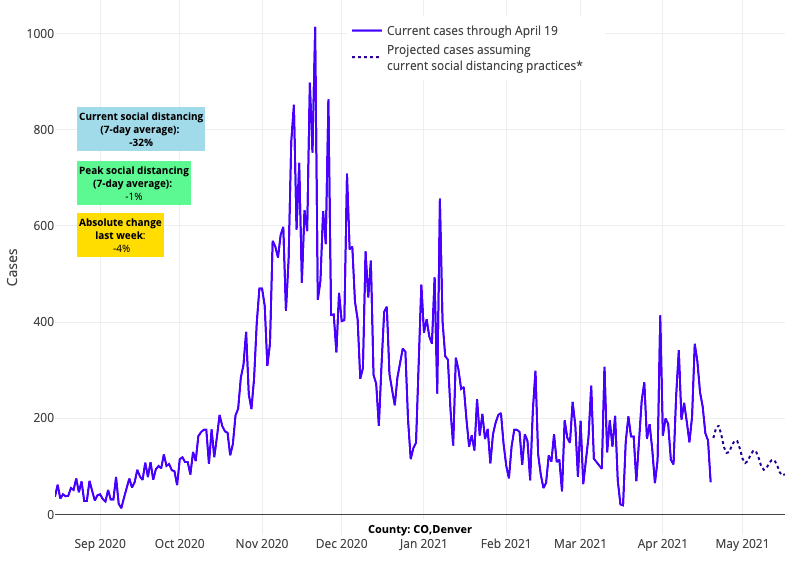
Above are the projections for Denver County in Colorado.
- The Southwest has thus far this spring resisted substantial increases in test positivity rates, reproduction numbers, emergency department visits, and hospitalizations, and our case incidence projections continue to remain flat across the region into mid-May.
- The region with the largest proportional growth in reproduction numbers and hospitalizations outside of Florida has been the Pacific Northwest. However, even as testing positivity rates have increased in many counties, they are starting from a much lower overall case incidence, and thus our models forecast flat growth in the coming weeks.
In our update last week, we saw emerging evidence of a shift in community transmission in many northern regions of the country, enough to suggest an inflection point had been reached for these communities. This change was paralleled by, and likely the result of, an acceleration in adult vaccine rates (at least partial vaccine rates) toward 50%. Although we noted concerns about increasing reproduction numbers in the South and along the Pacific Northwest and Atlantic coastlines, we were overall optimistic that the country was approaching a turning point for this surge.
After reviewing the data from this week and model predictions for the coming weeks, our optimism that the country as a whole has reached a clear turning point is further reinforced. As you can see above, fewer regions are experiencing growing case transmission. As such, we would anticipate that national case incidence estimates are likely to begin declining again, and hospitalizations will follow in tow. This is great news for a COVID-weary nation, but we are mindful that the rates of improvement for some areas will be quicker than others.
It’s time to begin vaccinating children and adolescents
All states have now opened up vaccination to children 16 and older—and are soon to offer Pfizer’s COVID-19 vaccine for children 12-15 years of age. Advocacy and education have been helpful to persuade vaccine-hesitant adults to obtain the vaccine; this now needs to be expanded to include recommendations for parents around vaccination of their children.
In that vein, we are increasingly concerned by some emerging commentary suggesting that there is less justification to vaccinate children than adults because the case fatality rate of COVID-19 is lower in children. Our team disagrees with those opinions and would emphasize the following:
1. Although most infections in children are mild and do not require hospitalization, the risk for mortality needs to be interpreted in the context of other pediatric illnesses for which we routinely vaccinate. Nearly 300 children have now died from COVID since last March. To put these numbers in perspective, we appropriately immunize children routinely for: 1) influenza, which accounts for about 200 deaths a year; 2) measles, which accounted for about 500 deaths a year before a vaccine was available in the early 1960s; and 3) varicella, which accounted for about 75-100 deaths a year before a vaccine was available in 1995.
2. Vaccines reduce morbidity from an illness, not just mortality. Measles and varicella caused much suffering and disruption in the lives of children and families prior to routine vaccination. COVID-19 can lead to multi-inflammatory syndrome in children or “MIS-C”—a rare but often severe and potentially fatal condition with unknown long-term effects that has affected more than 3,000 children in the U.S. The potential morbidity from MIS-C needs to be considered in the decision to vaccinate children.
3. Immunizing children for diseases that have more significant morbidity and mortality in adulthood has a long history. First, because nearly one-fourth of the population is children, vaccinating in childhood contributes to building population immunity. Furthermore, vaccinations for pathogens such as varicella, hepatitis A, hepatitis B, and human papillomavirus (HPV) are given in infancy for diseases that are more severe when they occur in adulthood. Also, as COVID-19 vaccinations increase among adults, children might become a more important reservoir for SARS-CoV-2, which would pose a threat to others at higher risk such as the immunocompromised.
4. Data from the first vaccine trial in adolescents support the efficacy of SARS-CoV-2 vaccination in children. Childhood vaccinations have long reflected the principle that more durable immunity is achieved in children, given that they have a more robust immunologic response than adults. In Pfizer’s clinical trial for vaccination of children ages 12-15, the vaccine was not only 100% effective, but also resulted in more significant antibody responses than were achieved in adults. As such, durable immunity may be better achieved through childhood than adult vaccinations. Additional investigation is needed and underway in children under age 12.
5. There are great costs to children and families from COVID-19 infection that extend beyond the infection itself. Many children benefit immensely from the social, emotional, academic, and physical benefits of in-person school and extracurricular activities. One of the values of influenza vaccination is that when protective, it can reduce days that children miss school and parents miss work. In the case of COVID-19, children will sometimes need to miss up to two weeks of school for even an asymptomatic infection or close-contact exposure, creating substantial child care gaps for parents. This can have significant financial impacts for the family and the community as a whole. This concern is likely magnified in large urban areas where disproportionate COVID-19 impacts have been common. Vaccinating our children will greatly reduce their infection rate and thus avert these important secondary consequences.
All told, we have now vaccinated more than 130 million individuals in this country, and scores more across the world. Evaluating safety and efficacy data are a critical part of this journey, and now six months in, the value of COVID-19 vaccination has exceeded expectations for its impact and safety. We are weeks away from authorization to begin vaccinating 12-15-year-old children, and we would strongly encourage families to participate in this next phase of vaccination. We look forward to trial results in younger children, which will help chart the course to more complete vaccination for all children in the future.
While a race is on to reach the end of the pandemic, there is a new race afoot that begins now. Vaccinating as many children as possible before the next school year provides an opportunity to ensure that schools fully return to normal in the fall, freed from the disruptions and negative impacts that COVID-19 has had over the last year. And that would be a welcome sight to see.
Paul Offit, MD, is the director of the Vaccine Education Center at Children’s Hospital of Philadelphia and a member of the FDA Vaccine Advisory Committee.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia, and is a co-author of PolicyLab’s Policy Review: Evidence and Guidance for In-person Schooling during the COVID-19 Pandemic.
