COVID-19 Outlook: Navigating School Reopenings During a Period of Sustained Community Transmission

Due to reporting delays in several states, in this week’s update to our COVID-Lab forecasting model we are unable to report on national averages for the reproduction number (a measure of transmission that indicates how many additional individuals could be infected by every positive case) or testing positivity rate. This limits our ability to interpret national trends. As such, we are focusing on regional updates in our weekly review of the findings:
- The reproduction number reached or exceeded 1 this past week in one-third of the 818 counties we follow in our model. This includes 8.4% of counties with a reproduction number over 1.25.
- Counties with the largest increases in reproduction numbers and testing positivity are concentrated in the Midwest, Mid-Atlantic and Northeastern states.
- Hospitalizations are now rising in 18 states, albeit at lower rates than they were in November and December.
The following are areas of specific concern:
- Michigan continues to sustain substantial transmission rates, particularly around major cities; reproduction numbers range from 1.16-2.02 across their counties, and testing positivity has increased, on average, from 5.1% to 7.4% in the last week. Since early March, hospitalizations have doubled in Michigan, and deaths, although well below winter peaks, are beginning to climb again. The largest growth in hospitalizations has been among adults between 50-64 years of age.
- Increasing reproduction numbers and testing positivity are apparent this week throughout Massachusetts, second only to Michigan in its abrupt change. Forecasts in the region have, therefore, projected increasing transmission in the weeks ahead, particularly in Barnstable County (Cape Cod), but also throughout Boston’s metropolitan area.
- Four of the five New York City boroughs and two of the city’s collar counties (Suffolk and Rockland) are among the 15 counties with the highest case incidence in the country (all over 300 weekly cases per 100,000 individuals). With growing test positivity, our models forecast weekly case incidence rates near winter peaks in the city; fortunately, the overall rate of hospitalization is still half of the winter peak.
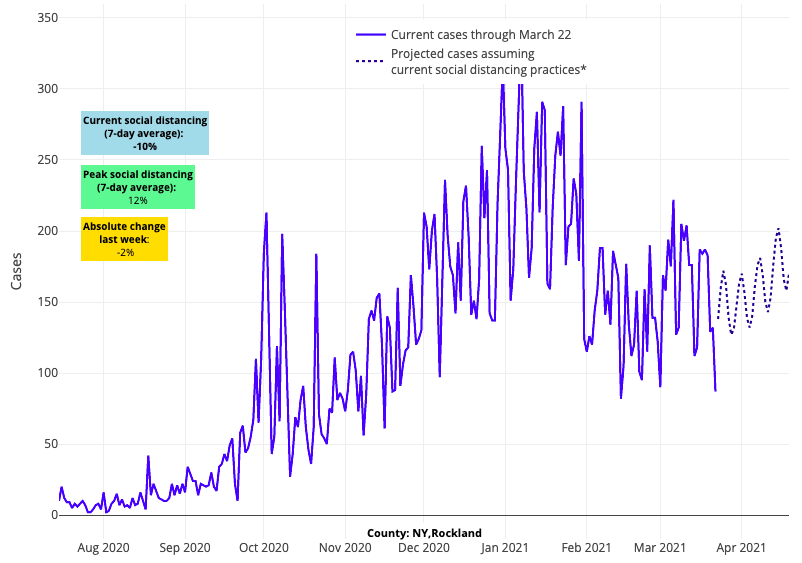
Above are the projections for Rockland County in New York.
- Case incidence and reproduction numbers in counties along the I-95 corridor between Washington and New York continue to increase, and our forecasts suggest these increases will continue over the next four weeks. Reproduction numbers are now exceeding 1.2 in the Baltimore and Philadelphia metropolitan areas and across counties in New Jersey.
- Reproduction numbers increased across Minnesota, Iowa, Illinois, Ohio and Indiana this week. Our projections for the Chicago area suggest increases in case incidence over the coming weeks that may be similar in magnitude to recent trends around Detroit.
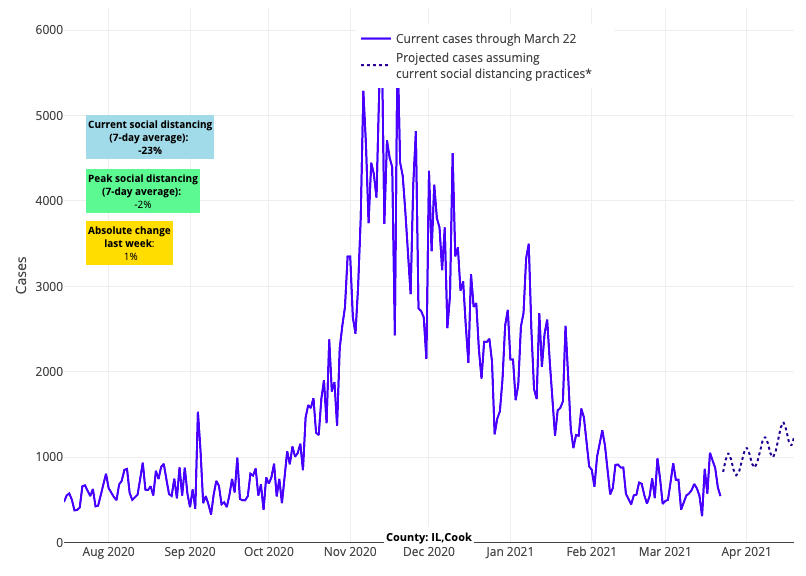
Above are the projections for Cook County (Chicago) in Illinois.
- Across the Southeast and Southwest we are seeing some increases in case incidence, but so far reproduction numbers have not substantially exceeded 1. However, both Florida and North Carolina are areas to monitor. In Florida, testing positivity is increasing in major metropolitan areas and emergency department visits are beginning to rise. In North Carolina, increases in test positivity and case incidence were evident in all cities this week; these numbers are projected to increase in the coming weeks.
Spring Resurgence Prompts Calls for Continued Vigilance
In reviewing local data this week, we are again concerned that improvements in case incidence and hospitalizations have stalled, or even worsened, in certain regions. Areas in the Midwest, Northeast, and Mid-Atlantic are of most concern as case incidence and reproduction numbers continue to increase. Michigan’s projections are particularly concerning, as the slope of the state’s case incidence has been steeper than other areas in the past two weeks, which has been associated with a substantial increase in hospitalizations. And our models project some additional growth in the New York City region that may reach peaks in weekly case incidence seen during the winter surge.
Despite these emerging hot spots, there are areas across the South, Southwest and Midwest that continue to experience improvements in their pandemic numbers. Texas, in particular, has shown resilience against increasing trends during recent weeks. The fact that some areas are worsening and some are improving leads to uncertainty as to the ultimate height and duration of this resurgence, or if resurgence will occur across all regions of the country. This uncertainty is likely the result of opposing forces in our communities that are either working to drive down case incidence (e.g., prior burden of infection, local vaccination rates, continued mask use, warmer weather) or potentially causing it to increase (e.g., relaxation of mask use, gathering in larger groups, increasing presence of variants).
Regardless of the state of any one region, the presence of relatively high virus burden in many locations suggest that the current resurgence will not dissipate abruptly. This should serve as a warning that communities that are still vulnerable should maintain vigilance as vaccinations continue.
Breaking Down the Latest Update to CDC School Guidance
The Centers for Disease Control and Prevention (CDC) this week updated its guidance for schools in spring. The new guidelines are accompanied by the release of new data from Salt Lake City and St. Louis suggesting transmission rates are low between school-based contacts when masking and other safety protocols are followed. The CDC guidelines permit full in-school instruction for elementary school students with 3-foot distancing in classrooms regardless of community incidence rates and allow for similar distancing between high school students when weekly community case incidence is below 100 cases per 100,000 individuals.
As full in-school instruction resumes, particularly if that requires reducing distancing between students, we encourage schools to be cautious and strengthen other in-school safety protocols in tandem.
It is important to note that some regions are seeing increasing infection rates again in children. This does not necessarily mean that linked transmission is occurring within schools that are repopulating. More likely, families are reducing their mitigation practices away from school; informal gatherings/parties and poor vigilance to safety protocols in youth sports venues are likely adding to this early spring resurgence. For communities where a “return to school” is the highest priority, restraint around other activities can more safely return youth into classrooms without the disruption that new cases can bring. If more students and staff arrive at school potentially contagious, the probability of a linked in-school outbreak increases. Sustained community transmission and spring break may, therefore, make a transition back to full in-school instruction challenging in some communities.
Those who carefully follow the challenges of studying COVID-19 risk in schools that have variably returned over the last year might also consider reading the CDC’s review of the evidence on school-based transmission. We welcome the accumulating data, but also must acknowledge its limitations. When headlines say a study proclaims “3 feet is safe,” for example, media outlets overlooked the limitations those studies had in drawing conclusions on that particular question. There is a natural tendency to confirm what you want to believe, which has been very strong throughout this pandemic the longer children have been out of school. Confirmation bias can be a powerful force that may cause one to overinterpret or overstate findings. We must also be cautious to over-generalize findings of studies from suburban or smaller districts and assume their outcomes would be replicated in large, urban school districts.
PolicyLab Releases Updated School Guidance
That said, as one reviews the entirety of studies, there is a preponderance of evidence that one can use to make a best-case assessment of the risk schools will face as they reopen more fully during a period of sustained case incidence. It is in this light that we are releasing our own updated school guidance highlighting the following key principles for school reopening that are best supported by the data:
- Safe in-school instruction is possible when students, particularly elementary-age children, are spaced as close as 3 feet apart in classrooms, assuming that other safety protocols, particularly masking, hygiene and symptom surveillance, are diligently followed. That said, our team preferred the previous guidance the CDC offered, which suggested distancing students by 6 feet “to the greatest extent possible.” We believe this recommendation recognized that schools could safely repopulate classrooms with less than 6 feet between students, but that maximizing distancing between students, whenever possible, is safest given the dynamics of COVID-19 transmission. This includes using flex spaces for learning—like gymnasiums, community buildings or outdoor fields—and being mindful of the additional risk posed during lunchtime when masks are down.
- While elementary-age children can return to full in-school instruction even when there are high levels of community transmission, the risk for outbreaks among adolescents in these same communities is likely higher. Even though data would support that younger children may be inefficient drivers of community transmission, adolescents are likely to transmit the virus similarly to adults even if their risk of severe illness is much lower. Therefore, outbreaks may be more likely to occur as high schools repopulate in communities with high transmission rates. That said, this risk can be variable and mitigated by a school’s attention to its safety protocols, with particular focus on compliance among students throughout the school day and during extracurricular activities.
- Higher community case incidence will increase risk of school-related outbreaks, but school-based transmission is unlikely to be greater than what is observed in other venues within the community. The CDC review cites numerous studies revealing that in the absence of safety protocols, linked in-school outbreaks are likely during periods of moderate or high community transmission. However, the review also notes that in the presence of strong safety protocols, trends in student and teacher case incidence neither exceed nor predate observed trends in the community. This is consistent with data from contact tracing that shows most infections occur outside of the school day. But the CDC review also reveals that the risk of school-related outbreaks grew as community incidence rose throughout the COVID-19 pandemic. We witnessed this phenomenon in our own region following Halloween, when school-related outbreaks occurred at a faster pace in November and December than other periods of the pandemic.
- COVID-19 testing can be a valuable addition to safety protocols as schools repopulate. Weekly assurance testing can both provide compelling data that schools are reopening safely and prevent contagious but asymptomatic individuals from conferring risk to schools or sports teams. Just this past week, the administration released $10 billion to support school-based testing programs for the remainder of the pandemic. For more information on testing, see our Project: ACE-IT webpage and our review of school-based testing programs.
- Youth sports are a venue in which there has been greater linked transmission than in classrooms, but risk can be mitigated through sensible attention to safety protocols. CDC guidance permits greater flexibility for outdoor sports; the data suggest that on-field play can safely occur with unmasked athletes, assuming their community is seeing declining transmission. However, this should not be viewed as license to abandon safety protocols limiting use of locker rooms, emphasizing strict adherence to masking off the field, and discouraging parties and gatherings when teams are not practicing or playing. Indoor sports should only be played without masking of athletes in the presence of frequent testing and low community transmission.
- The evidence on the safety of resuming arts programs and extracurricular activities is limited, but our team believes organizers can follow similar guidance as that for youth sports. As band or choir resumes in more crowded settings, keeping singers or students who play wind instruments at greater distances than others who do not play wind instruments is advised. Flexing to outdoor spaces, maintaining six-foot distancing, and adding weekly assurance testing can be valuable tools to removing risk from these activities.
With the release of our updated guidelines and modeling data this week, we are mindful that as much as all of us would like the pandemic to be over, many communities are likely to see sustained high transmission well into spring. The remainder of the school year will be beset with lingering challenges, particularly for communities that relax their guard. Those school communities that strengthen their safety protocols now will be best positioned to navigate the remaining months of this pandemic.
