COVID-19 Outlook: Schools Spring Forward

As we assess the latest batch of data from our weekly COVID-Lab forecasting model, we are encouraged to see that PCR testing positivity, case incidence and hospitalization rates are decreasing, on average, throughout the country. These continued declines are welcomed as the nation continues to ramp up vaccination efforts. Here are some specifics:
- PCR testing positivity rates declined nationwide to an average of 5.2% (down from 5.7% last week). Median reproduction numbers (a measure of transmission that indicates how many additional individuals could be infected by every positive case) also dropped, down from 1.05 last week to 0.89 this week.
- Improvements in case incidence rates continue throughout the Southwest and along the Pacific Coast. Our models project these improvements will continue in the major cities within these regions over the next four weeks.
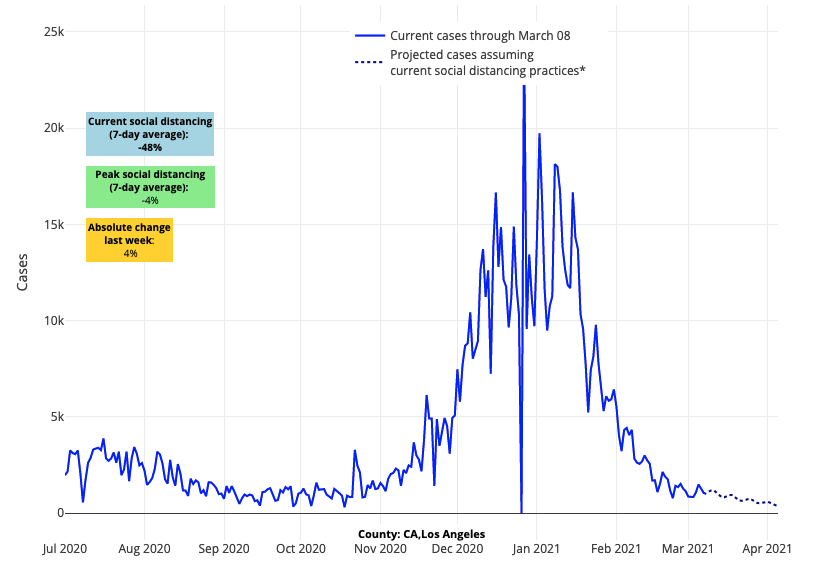
Above are the projections for Los Angeles County in California.
- In the Southeast, after several weeks of large decreases in PCR test positivity alongside improving case incidence, our models project continued declines in case incidence over the next month. Florida is the exception in this region (as we explain below).
- Hospitalizations of both adults and children continue to decline throughout the country, with about 40,000 individuals currently hospitalized for COVID-19 nationwide.
- The number of fatalities continues to decrease throughout the country. California and New York both dropped to fewer than 50 deaths a day this week. At their peaks, California had exceeded 600 deaths daily and New York had exceeded 150 deaths daily.
These reassuring national trends are countered with some regional areas of concern:
- Of the 818 counties we follow our model, 25% exceeded reproduction numbers of 1; this is up slightly from 20% last week. Much of these increases were concentrated in the Upper Midwest and areas of the Northeast.
- Reproduction numbers again moved above 1 this past week in New York City, where case incidence continues to be high, hovering between 250 and 400 weekly cases per 100,000 individuals. PCR testing positivity also increased last week in Manhattan and Staten Island. Our projections forecast sustained high case incidence with slow rates of decline over the next four weeks
- Declines in case incidence and emergency department visits have largely stalled throughout the major cities along the I-95 corridor from New York City to Washington D.C., and reproduction numbers hover near 1.
- In Michigan, reproduction numbers are again above 1. PCR test positivity rates are also up across most counties, including Genesee (Flint), Wayne (Detroit) and Macomb. The number of hospitalized patients in the state is climbing, albeit modestly so. Our models project increasing case incidence throughout Michigan in the coming weeks.
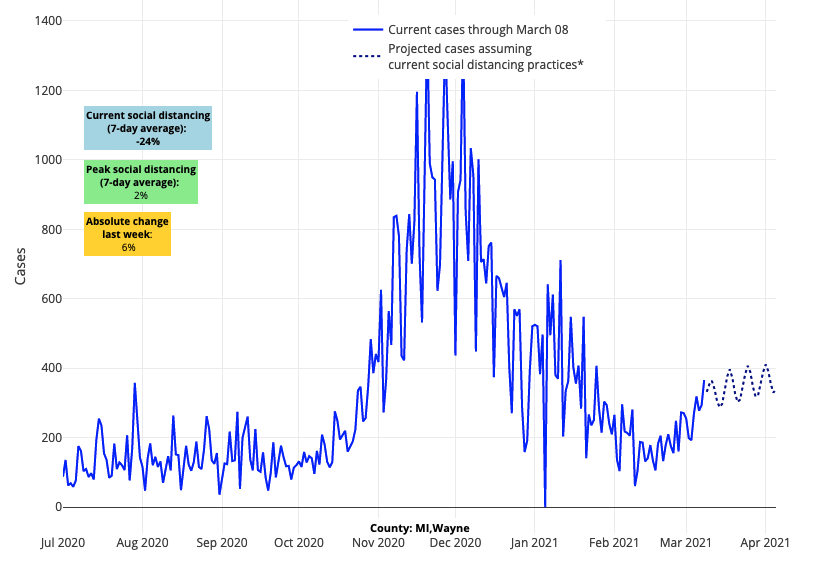
Above are the projections for Wayne County in Michigan.
- Case incidence continues to increase in the Denver area, and our models project continued growth in and around this major city in the coming weeks.
- While testing positivity has declined in Florida, declines in case incidence have slowed in the major cities, including Miami, Tampa Bay, Orlando and Jacksonville.
Why Are We Experiencing These Regional Variations?
As has been the case throughout this pandemic, case incidence, test positivity rates, and reproduction numbers are the products of a balance of factors that both foster and oppose virus transmission. While we have experienced progress over the past few weeks, the vacillation of these metrics at regional levels highlights the fragile nature of this process. Currently, some of the factors opposing transmission include warming temperatures and escalating vaccination rates. At the same time, overly ambitious reopening strategies, especially those that remove mask mandates, are likely stalling continued improvement and allowing for increasing transmission.
The fragile balance that we find ourselves in has led some to suggest that we should halt any progress towards normalcy. We would disagree. The number of cases among the eldest Americans has decreased in some locations that report age-specific rates. This improvement is likely multifactorial, but certainly has been aided by vaccination programs targeting this age group. This should help protect against a rebound of hospitalization rates even if case incidence were to again climb.
We also need to recognize that we can do many things safely as long as we are committed to mitigation efforts like mask use. Yes, we still have to be diligent and measured as we attempt to return to more activities, and no, we cannot throw caution to the wind by completely reopening communities and abruptly abandoning mask mandates. We also need to ensure that vaccination efforts increase, and that they are equitable across all communities given emerging data on growing disparities in vaccination rates across the country.
More Schools Are Reaching CDC Thresholds for Full In-school Learning
As disease burden continues to lessen in many regions, more and more U.S. counties are moving closer to the Centers for Disease Control and Prevention’s (CDC) thresholds for resuming full in-school instruction. We have seen large metropolitan areas drop well below 100 weekly cases per 100,000 residents, and our projections suggest those trends will continue over the next four weeks.
For the largest urban districts, like the School District of Philadelphia, this means opening for in-school instruction for the first time since last March. In general, urban school districts have had more significant barriers to reopening than suburban school districts, given the size of their school communities, the concentration of children within schools, older infrastructure, resource deficits, transportation challenges (many rely on public transit), and the disproportionate impacts that COVID-19 has had on their communities—particularly among families of color. Although the journey has not been easy, we are thrilled to see Philadelphia’s kindergarteners, first graders, and second graders arriving at schools this week, increasing vaccination rates among school staff, and the launch of a testing program that can provide teachers and high-risk groups of students access to weekly testing to further mitigate risk for transmission.
Other school communities that have been hybrid since last fall are now contemplating bringing all students back. Although school leaders, as per CDC guidelines, will try to maintain six-feet distancing among students “to the greatest extent possible” as more return, many recognize that they must reduce distancing between students to resume full in-school instruction. As they do so, we would encourage them to strengthen other layers of their school protocols, including retraining on appropriate masking by students and staff, holding more gatherings outdoors, and incorporating better testing programs that can maintain the viral burden within a school well below the surrounding community rates.
During this time, we would caution parents from concluding that slowed, or even increasing, community incidence should halt movement to in-school instruction. We have noted in prior blog posts that the CDC thresholds for school reopening are relative lane markers and must be considered alongside the risk tolerance of the school community and experience with school safety plans. We also advise closely monitoring trends in case incidence among children—more so than those of the community. In our region, that measure has remained flat among children, having improved substantially since the holidays (As of the end of February, Philadelphia’s was seeing 70 weekly cases per 100,000 individuals under the age of 20).
The Factors School Leaders are Considering as They Reopen
Throughout this pandemic, our team has accumulated tremendous respect for the unique decisions and challenges schools are confronting. While we offer guidance to many school communities, we are mindful that school leaders are incorporating evidence and guidance into a more complex planning process that includes many local perspectives on when and how to move to full in-school instruction.
From our conversations with school leaders, factors that they are considering include:
- Evidence of safety for in-school learning that has accumulated throughout the pandemic, particularly emphasizing reduced risk for elementary-age children (which was highlighted in recent CDC guidelines)
- Observations by school leaders and their communities of increasing student disengagement with virtual instruction since the holidays and accumulating impacts of isolation over the last year
- Growing vaccination rates of teachers and school staff
- Declining COVID-19 incidence, which our models project will continue as spring approaches, even as the rate of decline still remains uncertain
- Spring break, which is creating uncertainty for the potential of stalled declines in early April given how President’s Day weekend and other winter holidays contributed to community transmission
- Emerging evidence that school-based testing programs, for those that have access to testing, can both confirm that schools are maintaining no-to-minimal rates of disease transmission and further reduce the burden associated with asymptomatic infection
As school leaders weigh these factors independently, multiple paths forward have emerged. Some schools, for example, are choosing to return all students before spring break, so that they can acclimate to changes before the break and make adjustments as needed during the holiday week. Others have elected to repopulate incrementally each week to allow sufficient time for their staff to adjust to protocols. Still others have chosen to limit in-school instruction to elementary school students before the break and then return older youth a week past spring break. This latter approach can alleviate concerns from the holiday week itself, take advantage of warmer weather for outdoor learning, open middle and high schools during a period with likely even lower community transmission, and incorporate the lessons that are gleaned from the reopening of elementary schools.
Whichever approach a school uses to get more students back into the classroom, it is exciting to see many moving forward. It has been a difficult journey, but we are no longer trapped in a crisis that feels like it has no end, and we believe that the resilience of our youth will bring new optimism for our communities over the remainder of the school year.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia, and is a co-author of PolicyLab’s Policy Review: Evidence and Guidance for In-person Schooling during the COVID-19 Pandemic.
