COVID-19 Outlook: At the Height of the Pandemic, A Race Against Time
Below are the major findings from this week’s update to our COVID-Lab forecasting models:
- Reproduction numbers (which are a measure of transmission rates in an area) are up after the holidays to over 1.25 in 25% of the counties included in our model, indicating substantial viral transmission. Some of the highest reproduction numbers in the country are in Massachusetts, specifically the Worcester and Boston metropolitan areas. We also observed reproduction numbers over 1 across a vast region of the Upper Midwest, including in Minnesota and Wisconsin.
- Other areas of the Northeast continue to see increased viral transmission, particularly around New York City, where New York (Manhattan), Bronx, Kings (Brooklyn), Queens, and Richmond (Staten Island) counties are projected to have another doubling of daily cases over the next four weeks, having already doubled since the holidays.
- We’re also projecting growth in incidence into February for the Virginia and Maryland suburbs of Washington, D.C. Elsewhere in Virginia, a doubling in daily cases is possible over the next four weeks from Newport News through Norfolk and the Virginia Beach area.
- The proportion of ICU rooms currently utilized for COVID-19 patients (otherwise known as COVID ICU occupancy) exceeds 40% in Alabama, Arkansas, Georgia, Mississippi, North Carolina, South Carolina and Tennessee. This is occurring as our models are projecting a continued rise in case numbers for population-dense regions throughout these states. Specifically, we forecast daily cases will double over the next four weeks in the Atlanta metropolitan area, the major cities in North Carolina (Charlotte, Greensboro, Durham and Raleigh), and the shore locations of Myrtle Beach and Hilton Head Island in South Carolina.
- Florida’s COVID ICU occupancy has grown to 30%, alongside a steep rise in ventilator use and deaths that are now exceeding 100 per day. Our models project that daily case numbers could double in Jacksonville, Orlando and Tampa/St. Petersburg over the remainder of this month. Conversely, the current surge may be nearing its peak in counties across southeast Florida.
- Parts of Texas continue to be of concern. Over the last week, Houston has sustained a sharp increase in case incidence and hospitalizations have reached levels near the peak experienced this past summer. Unfortunately, our models project a continued rise in case incidence for Houston in the coming weeks, as well as in Austin, San Antonio and the greater metropolitan area of Dallas.
- The unrelenting transmission of COVID-19 in the Southwest continues to expand beyond California to across the Sun Belt. While our models suggest many counties in California are nearing their peak incidence, Arizona is now recording more than 100 deaths a day and we are projecting case numbers will increase in the neighboring mountain states of Nevada and Utah, specifically around Las Vegas (Clark County) and Salt Lake City (Salt Lake, Utah and Summit Counties).
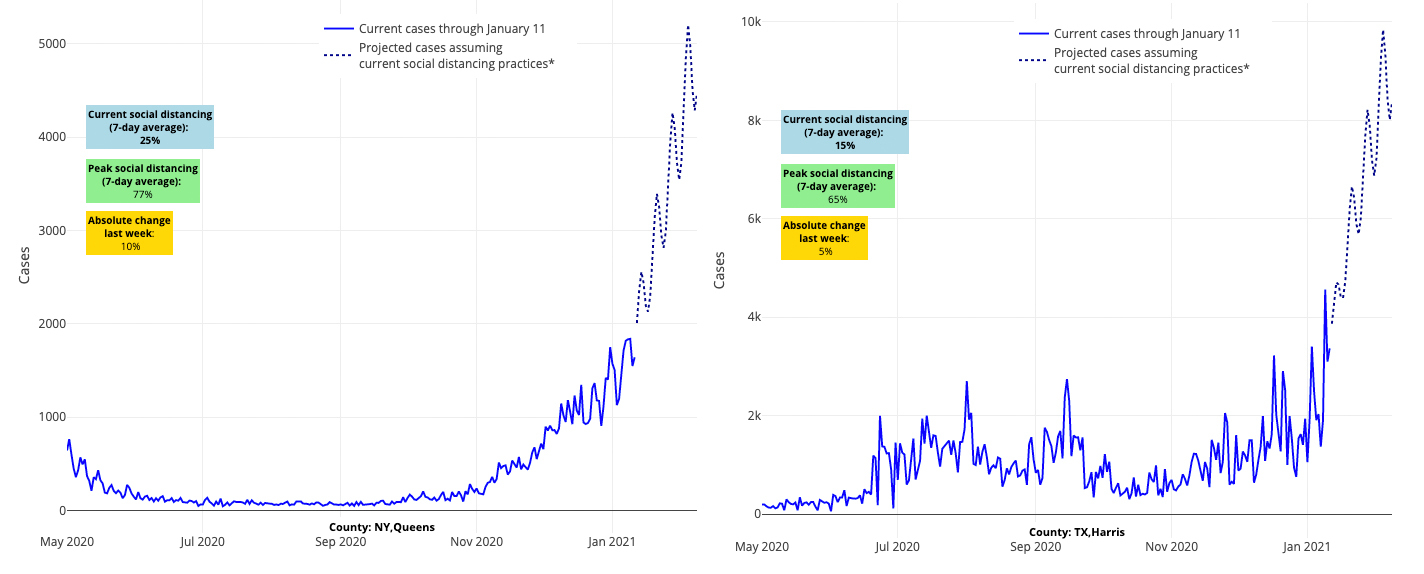
Above are the projections for Queens County in New York (left) and Harris County (Houston) in Texas (right).
Still, Signs of Optimism Emerge
The country may be reaching its peak incidence: Despite evidence for continued increases in local transmission in many of the counties our models follow, there are early signs that the country as a whole is reaching the peak of this current surge. Specifically, average PCR testing positivity was 15.3% across the country this week, which is an average decline of 1.2% from last week. Only nine states saw an increase in this metric last week, and of those, only California posted an absolute increase of more than 1%.
We’re seeing stabilizing or declining hospitalization rates across much of the country: Many areas in the Midwest, Ohio Valley and Mid-Atlantic are experiencing a stabilization or decline in hospitalizations despite growing case numbers. We are seeing similar trends in the Pacific Northwest. These trends in case numbers and hospitalizations are somewhat paradoxical, and bear continued monitoring, but there are many reasons why hospitalizations may be uncoupling from the growth in cases:
- Now a couple of weeks out from the holidays, intergenerational transmission borne from gatherings may be slowing.
- It is also reasonable to hypothesize that certain factors could result in increased transmission but decreased severity of disease. Perhaps more people are wearing masks given the high rates, thus reducing inoculums. Perhaps a novel variant first identified in the UK, while more transmissible, may not be as virulent as it proliferates.
- Finally, it is possible that as the vaccine reaches the most vulnerable, the spectrum of individuals who are being infected are younger and at lower risk for hospitalizations, thus easing the pressure on hospitals. We see some hints of this in North Carolina (see below), for example, where hospitalizations among older individuals have stalled.
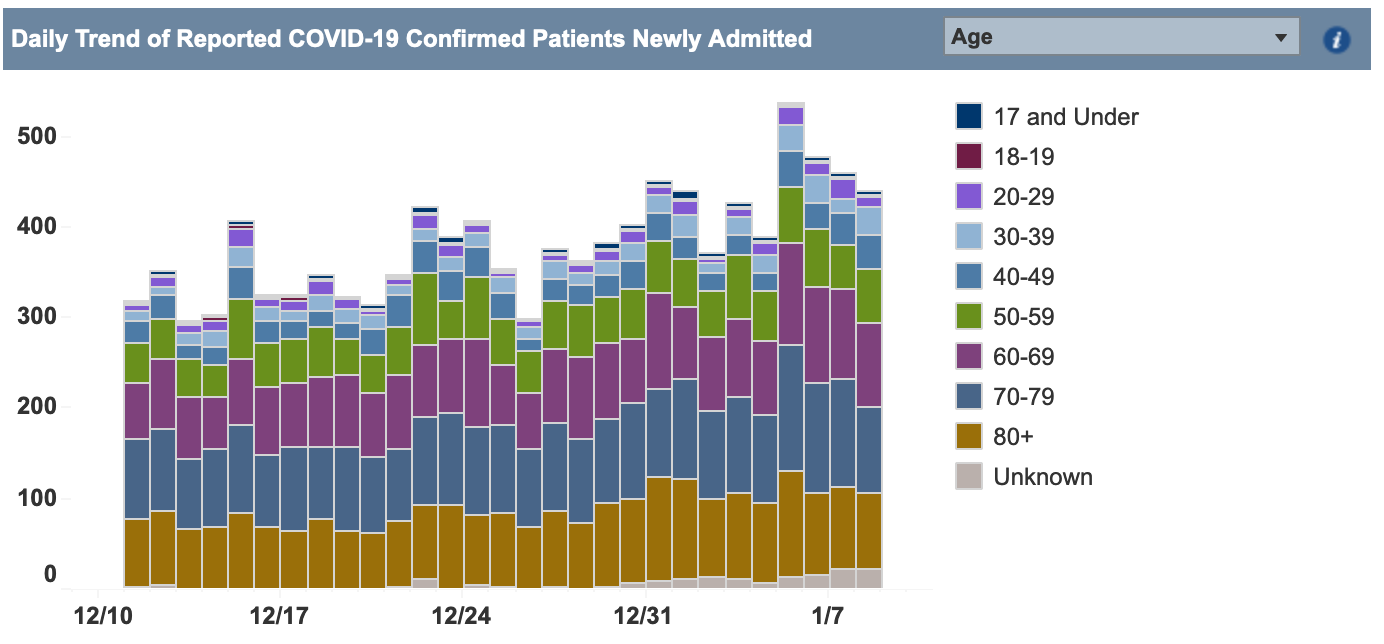
The graph above is sourced from the North Carolina Department of Health and Human Services.
Although we cannot determine the relative influence of these potential factors, the implication is the same: We are rounding a corner. While we are still at very precarious rates of infections and hospitalizations, and deaths are likely to lag at high rates for weeks, we are gaining some ground on our recovery from the pandemic.
School Guidance Around Testing and Vaccine Delivery
Our team continues to field questions about how schools might best navigate this phase of the pandemic, and this week we thought it would be helpful to review some of those questions that relate to increased testing and vaccine delivery—two key tools that can greatly improve school safety over the remainder of the school year. While the promise of these strategies is significant, there are hurdles of access and acceptability to both routine testing programs and vaccination. We encourage schools to partner with their local public health departments, health care systems, and other relevant local community agencies to garner greater testing resources, encourage staff participation and develop messaging plans to boost vaccine confidence.
Does weekly testing require full participation of school staff and high-risk students?
In our blog post last week, we highlighted a new program, Project ACE-IT, in the Southeast region of Pennsylvania that seeks to equip schools with protocols and resources for sufficient testing to reduce the risk of infection and increase confidence in the safety of in-person learning. The two main tenants of the program include:
- Rapid diagnosis of COVID-19 when individuals become symptomatic during the school day, expediting contact tracing efforts and targeted decisions about quarantine procedures from what they were in the fall
- Weekly assurance testing using rapid antigen tests for asymptomatic school staff and select groups of students, adding a low-cost option to identify contagious individuals earlier, providing even greater protection against unsuspected outbreaks. Anyone who tests positive will quickly be led to take a more sensitive point-of-care rapid molecular test (in our case through the CUE, a test that has been used by the NBA for assurance testing) to confirm that the positive antigen test was not a false positive.
Our team is reaching out to interested schools and their teachers throughout the region to encourage all staff and high-risk students to participate in Project ACE-IT, as the program ultimately works best with full participation. For example, if space constraints make it difficult for teachers and staff to distance while they eat lunch in a break room, weekly assurance testing could increase confidence in the safety of this important daily activity and, therefore, teacher and staff comfort in coming to school. Although negative tests don’t entirely exclude an individual from being exposed just before or after a test was done, the confidence in that situation, alongside other safety measures, is far superior than if half the individuals in the room had not been tested.
Assurance testing is, therefore, a commitment by a school community to protect each other. The fewer people who participate, the more penetrable the school becomes to transmission, particularly at the high rates we are seeing this winter, when more asymptomatic but contagious individuals may enter the school.
How soon until teachers will be vaccinated?
In communities across the country, the advocacy for school teachers and staff to be prioritized for vaccination has been heard. Following Centers for Disease Control and Prevention (CDC) guidance, state and local health departments have been prioritizing vaccinating health care professionals and residents and staff of long-term care facilities. But as we move to the second phase (known as phase 1B), other high-exposure workers and high-risk residents are now in line to receive the vaccine. However, this group—comprised of older individuals, as well as police, fire department and other essential workers—is much larger than the first. Teachers are among this larger group and, assuming challenges in supply chain continue, we can anticipate that the full vaccination of school staff may play out over the next two to three months at best (noting that the vaccine requires two doses for full effectiveness, separated by 3-4 weeks).
This makes it critically important for schools to work with their public health departments now in order to identify how staff will be vaccinated.
Addressing individual staff risk early can help avoid shortages of teachers for in-school instruction that plagued many schools in the fall. We have also learned that certain staff positions within schools confer increased risk that should be equally considered. Here are a few examples:
- School bus drivers have faced disproportionate risk of transmission on buses where social distancing could not be achieved. Offering them the vaccine first recognizes that risk. Additionally, by keeping bus drivers healthy and available for work, a community can help ensure that children can get to school each day.
- Staff working with children with special needs who cannot mask or maintain distancing during the day also face increased risks.
- Finally, recognizing that transmission among older youth has been an impediment to keeping high schools open, prioritizing high school staff for vaccination is advised.
Using this type of criteria to order the recipients of vaccines can help insulate schools from the ups and downs of community transmission in the weeks and months ahead. And it will ultimately pave the way for more students to return for in-school instruction. We are mindful that vaccine hesitancy and mistrust are critical issues to overcome, particularly among historically marginalized populations, and sufficient education and messaging will be required to encourage full participation in vaccine receipt. So, beyond the logistics of vaccine inventory and distribution, there is a much larger process of preparing for vaccine receipt that is necessary for all schools to undergo now if they wish to safely welcome more students into school buildings this spring.
In a week in which we are seeing the highest rates of the pandemic, the urgency of testing and vaccine rollout cannot be overstated. In an email with our state and federal partners announcing the launch of Project ACE-IT, Dr. Kristen Honey, U.S. Department of Health and Human Services’ chief data scientist and one of the unspoken heroes that made our program possible, remarked that “COVID response is a team sport.” At a time of national tragedy, we are encouraged to see people coming together every day to work through these challenges as a team, contributing to a gathering momentum to change the course of this pandemic.
