COVID-19 Outlook: Returning from the Holidays Beset with New Challenges, and New Solutions

We began to see early evidence last week that travel and gatherings during the holiday season translated into increased transmission, as COVID-19 cases and hospitalizations predictably accelerated across the country. Sadly, this week’s data confirms these trends. Below are the topline findings from this week’s update to our COVID-Lab forecasting model:
- Testing positivity rates are exceeding 15% across the country this week; the 10 states with the greatest increases in testing positivity include Alabama, Arizona, Iowa, Kansas, Louisiana, North Carolina, Oklahoma, South Carolina, Tennessee, Texas and Utah.
- Testing positivity is up in many parts of the Northeast, with the greatest increases in testing positivity and transmission rates in New York state. Our models are predicting that daily cases may double in most New York City boroughs within the next four weeks.
- PolicyLab’s models project case numbers to grow well into January in the Washington, D.C. metro area, led by the Virginia and Maryland suburbs.
- Testing positivity and case incidence continues to surge in the Southeast. For example, we project case incidence to double during January in the metropolitan area of Atlanta. Furthermore, ventilator use is up 60% in Georgia in the few short weeks since Christmas.
- Our model’s projections for case incidence over the next four weeks in southeast Florida exceed peaks seen earlier this summer. Across Florida, the number of COVID-related emergency department visits sharply rose after the holidays and the state is now recording 100 deaths daily.
- Our case incidence projections for Dallas, Houston, San Antonio and Austin show no signs of slowing in the coming weeks. These forecasts come as Texas climbs to 45% COVID ICU occupancy and 200 deaths a day.
- In the Sun Belt, Los Angeles continues to hover near 1,000 cases weekly per 100,000 individuals and testing positivity in the city has remained very high, approaching 30%. Fortunately, our model projects Los Angeles is near its peak, with areas of San Francisco and Sacramento being a week or two behind. Maricopa County (Phoenix), Arizona is nearing 700 cases weekly per 100,00 individuals, but the rate of growth has slowed.
- Concerns are growing for the Pacific Northwest, as some of the highest transmission rates in the country were observed in the state of Washington this past week. According to our model, the Seattle region is at risk of seeing cases double over the next few weeks.
- Despite increasing test positivity and some modest projected case growth throughout the Midwest, including in Chicago and Detroit, there continue to be improvements in emergency department visits and hospitalizations.
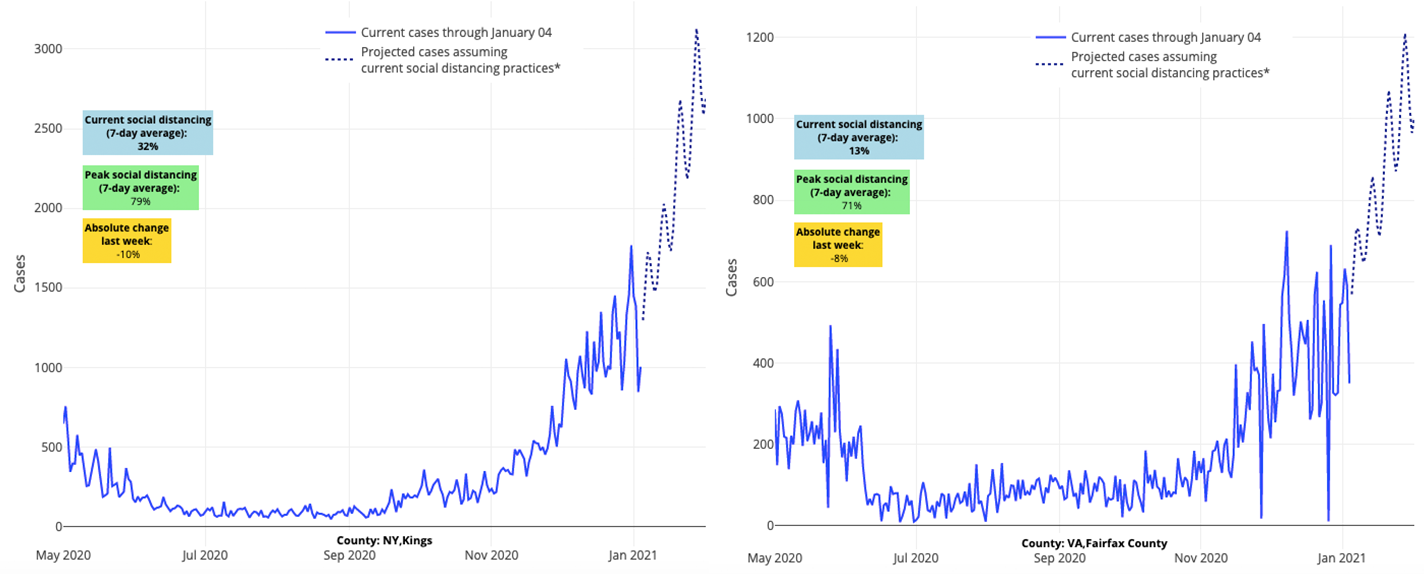
Above are the projections for Kings County (Brooklyn) in New York (left) and Fairfax County in Virginia (right).
Implications of the Emerging SARS-CoV-2 Variants
The fact that cases are spiking in the New York City region, and will continue to rise according to our model, piqued our interest regarding the emerging variants of SARS-CoV-2, particularly the one first detected in England that may spread more easily. Certainly, the city’s case growth could be attributed solely to gatherings around the holidays, but this variant was detected in Saratoga Springs, New York this past week. The unusual pace of growth in New York City is now matching similar outlier growth in the Saratoga area.
As interest in this novel variant grows, we encourage our readers to reference content from the Centers for Disease Control and Prevention (CDC). All respiratory viruses develop mutations as they replicate, resulting in variants, and there have already been numerous variants identified during this pandemic. The concern over this particular variant is the potential for increased transmission. As we wait for additional data, we can be confident in the fact that there is no evidence that this variant results in more severe disease or increased risk for death. That said, we should assume that this variant is present in many regions across the U.S., and the potential for increased transmission should strengthen our commitment to the well-known and effective mitigation strategies of masking and social distancing. Further, this is likely not the time for policymakers to reduce current restrictions.
How Should Schools Navigate the Coming Months?
The continued growth of case incidence on top of already high case rates in many areas of the country is occurring as many schools prepare to reopen this month. As disconcerting as the case numbers are in early January, we remind ourselves that schools are better equipped to navigate the coming months than they were in the fall.
As schools consider their options for returning to in-person schooling, we recognize that there is not a “one-size-fits-all” approach. Many schools are electing to remain virtual for the first week or two of January to allow the case growth from the New Year’s weekend to abate. Others, armed with staff educated by the challenges they experienced and multi-layered protocols that they implemented and refined this fall, are opting to return to the classroom more quickly. These schools often have larger campuses and/or smaller student enrollment, or are in districts with strong relationships with local health departments.
If we learned anything from the fall, it was not to underestimate the motivated school or school district. Each school has its unique circumstances, and motivated communities and school districts can have success in both reopening schools and keeping members of the school community safe.
That said, each district is having to consider the delicate balance between the virus’ risks and the consequences of additional time away from in-person learning. Yes, January presents a whole new set of risks. The number of schools experiencing apparent school-related clusters and outbreaks in the fall grew as community incidence rose, both in the U.S. and in Europe. However, we can learn from and be reassured by some of the knowledge that we garnered during those outbreaks. For example, student-to-teacher transmission was much less frequent than transmission between students, or between staff members. We also learned that elementary schools saw fewer outbreaks than high schools; many school districts were able to keep elementary schools open, even as high schools were shuttered in advance of winter break.
The presence of the aforementioned SARS-CoV-2 variant that may be more transmissible does need to be considered in assessing the risk-benefit ratio of returning to school. Officials in England made the difficult decision to close its schools this week as they noted a greater proportion of cases among kids in their current surge and as they approached hospital capacity. As we plan a return to school in the U.S., it will be important to monitor the growth of cases among children. At the very least, the existence of this new variant should serve as a reminder that the multi-layered safety protocols that helped schools navigate the fall will be even more critical for in-school instruction over the winter and into the spring.
Given the uncertainty of the new variant strain and high transmission rates we are still seeing after the holidays, we encourage schools to seek the middle ground and regain the footing they held from fall. This is not the time to be bold in repopulating classrooms; that time will come later toward spring once vaccine distribution has fully reached school staff and as warmer weather ushers in lower transmission rates. But even if January is not the moment to be bold, there is opportunity to support schools to at least in part return children to in-school instruction.
The delays of reverting to in-person schooling have been most disruptive to larger, urban public school districts with schools in low-income and densely crowded communities. The stubborn inequities faced by under-resourced communities, including greater rates of transmission and disproportionately high rates of hospitalizations and deaths, have in part informed many of their decisions to keep school doors closed. We understand the concerns among the school staff in these areas when it comes to in-person schooling. However, there are examples of public and independent schools that have successfully made this move, and we should look to them for guidance. Our goal as we enter the second half of the school year is to facilitate the availability of additional tools (i.e., access to vaccines and diagnostic testing) that will allow more schools to achieve comfort in safely reopening their classrooms and, importantly, aid in building confidence and trust among members of the school community.
Preparing for the Vaccine
We’re grateful that the vaccine has already been safely administered to millions of essential workers across the country. In the coming weeks to months, we need to commit to efforts that bring protective vaccines to school staff. Providing school employees with this layer of protection will allow us to be even bolder in returning to full in-school instruction later this spring.
Our team has joined others in advocating for school staff to be designated as essential workers, thus prioritizing them for early vaccine access in the coming weeks. Even when our vaccine supply is sufficient to begin vaccinating school staff, schools will face the logistical challenges of administering vaccine to eligible staff as quickly as possible. Now is the time for schools, with support from public health departments, to build their vaccine distribution plans and, just as importantly, to begin communicating these plans with their school community. Additionally, school and public health department leaders will be faced with the need to build trust among school employees who may be hesitant to receive the vaccine. Beginning conversations early, in partnership with trusted health professionals and community organizations, will benefit schools in ensuring rapid and equitable uptake of vaccines upon their arrival.
The Value of Increased Testing: Project ACE-IT
While schools await the vaccine, we must recognize that distribution challenges and the requirement for two doses of the vaccine over 3-4 weeks will inevitably stretch the process of vaccinating staff into the early spring. In the interim, initiating in-school diagnostic testing for staff and students can add another layer of protection that was not widely available earlier in the school year. From a recent study Dr. Rubin helped conduct, we have learned a lot about the value of assurance testing in colleges. Weekly, or sometimes biweekly, testing of all college students allowed some campuses to minimize transmission among its students and protect the wider community around them.
This week, we are proud to introduce Project ACE-IT (Advancing Childhood Education through Increased Testing) to southeast Pennsylvania, a school-based testing program. The two components of the ACE-IT strategy are:
- close partnerships between municipal health departments and school districts to offer in-school testing of symptomatic students and staff, and
- weekly testing of staff and select groups of students.
This program, operationalized by county health departments and local school districts in consultation with members of our PolicyLab team, has been facilitated by access to point-of-care testing from the CDC and the U.S. Department of Health and Human Services. Through it, we aim to more rapidly and comprehensively test symptomatic individuals in schools to hasten contact tracing, guide decisions about classroom quarantines and minimize unnecessarily prolonged school absences. Additionally, Project ACE-IT seeks to perform weekly surveillance testing of school staff with the intent of detecting adults in school buildings who have been infected with SARS-CoV-2 but are not yet symptomatic, potentially avoiding additional transmission within the school. Limiting spread within the school should help make buildings safer and, most importantly, reduce the type of outbreaks that shuttered classrooms throughout the fall.
As we embark on this program, we are thankful for the support from our leaders in Washington D.C., Harrisburg, local health departments, intermediate units and school districts that have worked tirelessly to make this testing plan a reality. There is still much work to be done, and we will update you as we enroll schools from Philadelphia and the surrounding counties throughout the coming weeks. Nonetheless, we are grateful for the efforts thus far that have unified many people with a common purpose—to return more children to school as the new year begins.
And with that, we welcome 2021.
Deanna Marshall, MPH, is a former research associate at PolicyLab.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia, and is a co-author of PolicyLab’s Policy Review: Evidence and Guidance for In-person Schooling during the COVID-19 Pandemic.
