COVID-19 Outlook: Time to Preserve Our School Reopenings As a New Wave Moves In

Our team has been doing these models since March, and we've had many concerning weeks, but we would put this week's forecasts among the most concerning we've seen.
Following a long-awaited pause in COVID-19 transmission over the past few weeks in many areas of the country, the surges in the Upper Midwest and Mountain States that we reported on last week are now evolving into outbreaks sweeping into Michigan and Indiana, and increasingly into Illinois. The Pacific Northwest is worsening again, and we are seeing the early footprints of resurgence in the Northeast, particularly in New York, where testing positivity rates are up throughout upstate and Rockland and Kings (Brooklyn) Counties are experiencing significant outbreaks.
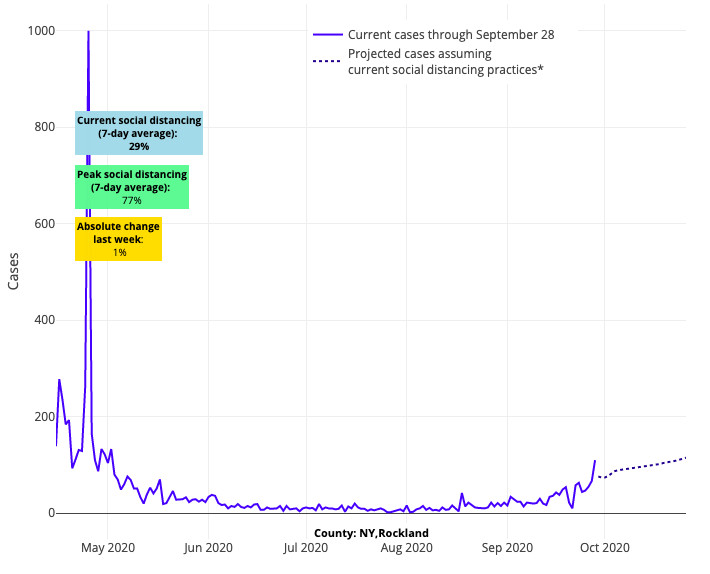
Above are the projections for Rockland County in New York.
While New England is, by comparison, relatively stable, we are monitoring modest increases in testing positivity rates in Connecticut, Rhode Island, Massachusetts and New Hampshire. And in the Mid-Atlantic, New Jersey once again has widespread transmission risk along its shore and our forecasts have worsened for central and south central Pennsylvania.
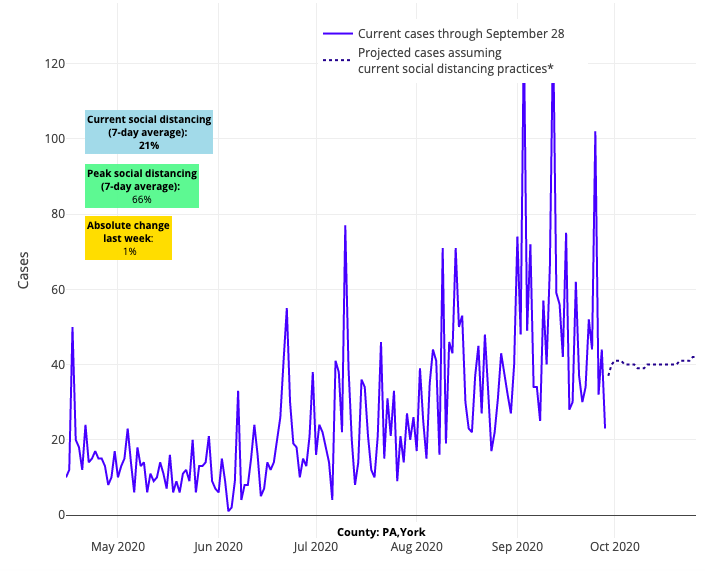
Above are the projections for York County in Pennsylvania.
All of this is signaling that the anticipated negative consequences of cooler temperatures, is happening more quickly than we thought, possibly accelerated by fatigue in committing to mitigation strategies within our communities. What we are observing is validating our published research and forecast models from the early spring demonstrating that colder, drier weather can contribute to more efficient transmission of SARS-CoV-2. Of additional concern are the rising hospitalization rates in parts of the Upper Midwest and Mountain States. There is reason to believe that increased hospitalizations will follow in the coming weeks for other areas currently experiencing greater caseloads.
The real question now is whether state leaders have the fortitude to act quickly to try to hold the line. Decisions by leaders should be made with the ultimate goal of protecting communities that are beginning to open schools for in-person instruction. This could mean conceding certain events outside of school, like sports, unless widespread, rapid testing is available to allow those activities to proceed safely. We should also be extending bar closures, limiting gathering sizes and strengthening enforcement of masking mandates in advance of this potential next wave in our northern cities.
Some might question whether opening schools at a moment when another wave is forming makes sense. But for those areas that have worked hard to mitigate the virus, they are still positioned to open schools under well-developed protocols, as we’re seeing increasing evidence that school safety plans are working and transmission risk within the school itself is low. We are forging ahead with helping schools in regions with low community transmission rates get kids back in the classroom while the safe window still exists. This includes providing evidence to help strengthen the plans that schools have been preparing since the spring to keep students, teachers and staff safe.
We would like to unpack these protocols a bit more for you because our compliance with them will likely determine how long we can continue in-person schooling. Here are some common questions we are receiving, and the answers we are providing:
1) Given that it is unrealistic to assure children will reliably wear masks and stay six feet apart (particularly younger children), aren’t the protocols flawed?
This has been the most common question we’ve received, whether for masking, distancing, or even the screening of children for exposure or symptoms before they come to school. Our answer emphasizes the multi-layered public health approach that is being pursued, by which multiple failures would need to occur for an outbreak to originate in a school building. If a school opens during stable community infection rates, and most of the students are reliably wearing masks, social distancing for much of the day (or within six feet only for brief stretches), and carefully screened out from school attendance when they are sick, then we can hope that transmission will be limited. Notably, the evidence that has accrued on school transmission risk to date has validated the success of these protocols in mitigating secondary transmission. That teachers are reliably distanced and masked most of the day as well should increase confidence that their chances of becoming infected are small. It’s only when we introduce risk, such as through unregulated sports activities or group, unmasked gatherings, that the risk increases for both students and teachers.
2) What if we can’t achieve all of the safety recommendations?
Because a multi-layered public health approach is central to our guidance around mitigation strategies, schools have the opportunity to boost some interventions when they cannot achieve others. For example, a common concern has been the limited bus availability to safely transport students in larger public school districts while maintaining social distancing. Crowding on buses for an extended period of time during the winter viral season is a high-risk moment for school-related outbreaks. In this scenario school districts could enact other mitigation measures, like assigning seats on the bus, grouping together siblings and cohorts that live near and spend time with each other. Volunteer bus monitors could screen children for symptoms before getting on the bus and assist the bus driver with ensuring students wear their masks while in transit. Bus windows can remain open for better ventilation, and parents can be encouraged to help their children practice good hand hygiene before and after riding on the bus.
All told, a layered approach—boosting some mitigation strategies while others cannot be fully deployed—is the essence of a public health-tiered strategy that should protect our students, caregivers and teachers through this academic year.
3) As the White House releases new rapid tests this week, should schools be a priority?
The short answer is absolutely, yes. It is our understanding that the White House Coronavirus Task Force has prioritized students in K-12 as a target population for antigen testing to preserve the ability for in-person learning and limit transmission to other vulnerable members in the community. But how you implement comprehensive testing for students and teachers is a whole other question.
While there will not be enough tests to universally and continuously screen all students and staff, we should avoid temptations to only do random spot testing at infrequent intervals. That is infection control theater and does little to mitigate risk. Rather, we would recommend prioritizing testing for scenarios during highest-risk moments for transmission in schools. For example, there is a critical need to return children with special education needs to the classroom, given that they cannot reliably learn through virtual learning. But these classrooms often involve high-touch engagement in close environments, and some students may not be able to reliably wear masks or face shields. Providing frequent screening through both symptom surveillance and regular testing may be a reliable strategy to assure safety in these classrooms. In a similar fashion, daycare, pre-K, and kindergarten settings are inevitably challenged by inability to fully embrace distancing and masking. Providing regular screening to teachers and students in these locations would confer additional safety and reassurance, even while recognizing that the risk is lower of symptomatic infection and transmission among our youngest children.
Finally, the return of sports and extracurricular activities (such as music and theater) has been controversial for many schools as they reopen. Our team understands that, despite the very appropriate concerns of public health officials regarding documented outbreaks linked to these activities, they provide important physical, emotional, and social benefits to children and their communities. Multi-layered approaches discussed above for return to school can be similarly effective in returning to these activities. For example, having students wear masks as much as possible during practice and warm up and not on the field of play. The addition of frequent testing can also help mitigate these risks to acceptable levels. For high-contact sports (such as football, basketball and ice hockey), through which transmission risk may be higher, implementation of rapid testing on top of other mitigation strategies can provide adequate safety.
Flying blind without implementing strong mitigation and testing strategies in communities that have permitted sports and arts activities to return is a sure recipe for driving more transmission—which will ultimately threaten the ability to keep kids in school.
4) Is there any flexibility in the 14-day quarantine following school-related exposures?
There is a great need for more nuanced approaches to handle non-household exposures for teachers and staff who are a part of our essential work force. Quarantine of students and teachers who are exposed for more than 15 minutes in close proximity to others who test COVID-positive, or who may have been exposed during a sports or arts activity, is an important component of every school’s safety protocol. But, availability of rapid testing has the potential to return teachers and students to school in a timelier fashion. Eighty percent of symptomatic SARS-CoV-2-positive patients will develop symptoms within a week. Knowing this fact, pairing a 7-day quarantine with a subsequent negative SARS-CoV-2 test would mean that the exposed individual would be extremely unlikely to be infected. As such they could return to work or school, while masked and practicing social distancing, with little risk to those around them.
We are learning more and more about school-related COVID-19 transmission every day. But we also recognize that the greatest test is ahead, as impacts of the winter respiratory season are already starting. Time spent now fortifying school protocols, and taking advantage of the benefits of new tools like rapid testing, can prepare for the journey ahead and blunt the additional risk that cold weather will bring. Hopefully, with a bit of resilience in our schools, we can overcome the challenges in our way until a safe, effective vaccine arrives.
Gregory Tasian, MD, MSc, MSCE, is an associate professor of urology and epidemiology and a senior scholar in the Center for Clinical Epidemiology and Biostatistics at the University of Pennsylvania Perelman School of Medicine. He is also an attending pediatric urologist in the Division of Urology at Children's Hospital of Philadelphia.
