COVID-19 Outlook: A Summer Resurgence as Schools Plan for Fall
As COVID-19 incidence rates decreased in late spring 2021, our team stopped providing weekly COVID-Lab blog updates but noted we would return at key moments in the months ahead. This week, almost three weeks after a July 4th holiday that signaled a near full reopening of our country, our team returns with a blog update alongside the release of our 2021-22 school guidance for K-12 education. These resources are accompanied by current national trends for case incidence informed by data provided by the Centers for Disease Control and Prevention (CDC) and the U.S. Department of Health and Human Services (HHS). Although we are no longer publishing county-level projections on our website, we are still reviewing county-level models, some of which we will highlight in this post.
Here are updates from this week’s data:
- Across the 821 counties in our model, average testing positivity has once again eclipsed 5% (now 5.1%), up 1.3% since last week.
- Testing positivity rates vary substantially by county, but 20% of counties are now above a 9% test positivity rate. States with higher test positivity rates are concentrated in the South and Midwest, including Nevada (14.9%), Oklahoma (12.6%), Missouri (11.2%) Mississippi (11.1%), Alabama (10%), Utah (9.6%) and Arkansas (9.1%). Texas, Louisiana, Kansas, Arizona and Tennessee are quickly approaching a 9% test positivity rate as well.
- The average reproduction number (a measure of transmission) for the country has increased to 1.60. Nearly two-thirds of all counties have higher transmission than last week and a majority have reproduction numbers over 1.25.
- Outbreaks are now highly regionalized and skewed; 17% of counties are above 100 weekly cases per 100,000 individuals, and 4% are above 200 cases per 100,000 individuals. These latter areas include Springfield, Mo. and Little Rock, Ark., which have led the country in the summer resurgence. Metropolitan areas with high case incidence are expanding and now include Jacksonville, Fla., the wider metropolitan area and I-10 corridor west of New Orleans, La., Jackson, Miss., and Las Vegas, Nev.
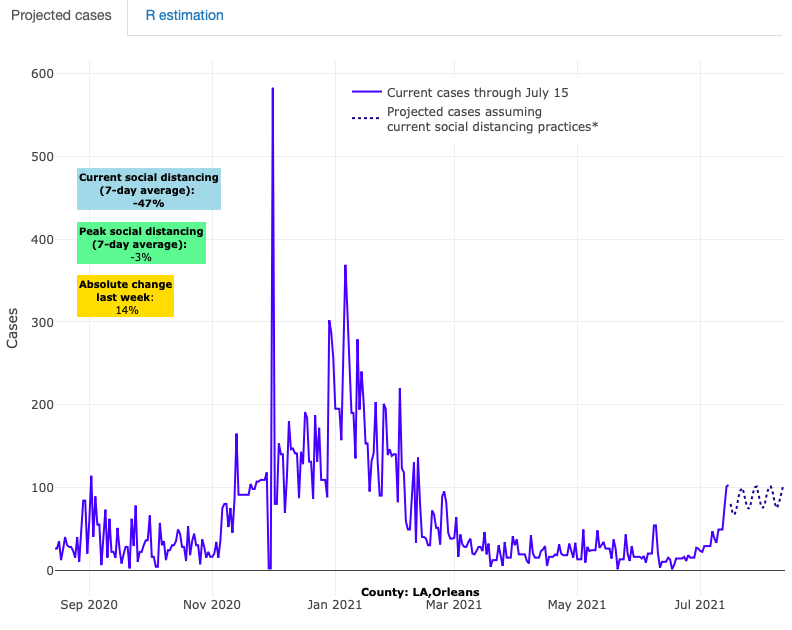
Above are the projections for Orleans County in Louisiana.
- Resurgence in the South is becoming more widespread. Most concerning is Florida, where overall vaccination rates are still below 50%, and where over the last week tests conducted increased by 30% and PCR test positivity climbed by an absolute 3.5% to 10%.
- While areas of the South continue to demonstrate potential for sustained or elevated transmission in the coming weeks, areas throughout Missouri may be nearing or moving past their peaks in transmission. That said, recovery may be slow with sustained and elevated transmission for several more weeks.
Taking stock of a summer resurgence
As seen over the last year in our modeling, it typically takes about two to three weeks to see the impact on COVID-19 cases of points in time when people might gather (e.g., holiday weekends). Now, three weeks after the July 4th holiday, we are witnessing resurgent summer COVID-19 transmission around the country. No county has been spared in this current increase in transmission. Even in the North, where cases have remained relatively stable since late winter, transmission spiked in every major city.
However, the growth in transmission and hospitalizations are most striking in areas of the Midwest, South and Mountain states. Case incidence in some counties in our forecast is eclipsing 200 weekly cases per 100,000 individuals; it was late winter 2021 when we last experienced these incidence rates. This increase has included severe cases requiring hospital admission. Hospitalizations have more than doubled in Arkansas, Missouri, Nevada and Utah. In Florida, for example, hospital census increased very quickly from less than 2,000 adults hospitalized to nearly 3,000 adults hospitalized since the end of June.
While such increases can bring anxiety, they should not come as a surprise. Larger gathering events inclusive of unmasked attendees have returned, and many Americans are traveling for summer vacations all the while leaving mitigation measures behind. Additionally, significant resurgence is most apparent in areas with lower vaccination coverage. Viruses will find the path of least resistance; SARS-CoV-2 is no different and currently the path of least resistance for SARS-CoV-2 is through the unvaccinated.
In Missouri, for example, we have seen higher COVID-19 incidence rates in Springfield (Greene County) than in Kansas City (Jackson County), while rates in Kansas City are higher than in St. Louis (St. Louis County). What differentiates these three metropolitan areas are the community vaccination rates: Only one-third of residents in Springfield are fully vaccinated, compared to 40% in Kansas City, and nearly 50% in St. Louis. We are seeing similar patterns in other states. For example, in Jacksonville, Fla., less than half of their population is vaccinated; that same community is nearing 20% PCR testing positivity and is exceeding 200 weekly cases per 100,000 individuals.
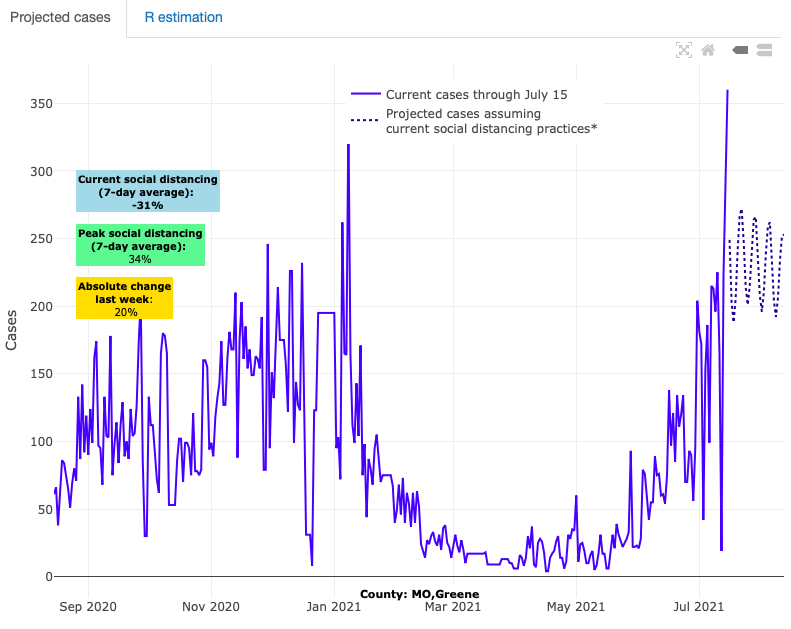
Above are the projections for Greene County in Missouri.
Conversely, counties with the highest vaccination rates—those exceeding 70% of individuals over 12 years of age who are at least partially vaccinated—have been insulated from the substantial increases experienced elsewhere in their states. This includes Cook County (Chicago, IL), Fairfax County, VA outside of Washington, D.C., and Madison, Wis., where case incidence is at or below 20 weekly cases per 100,000 individuals, and Raleigh, N.C., where case incidence is at 35 weekly cases per 100,000 individuals. Most importantly, the cases of COVID-19 in the areas with higher vaccine coverage tend to be mild in severity. This is evidenced by relatively low hospitalization rates in these areas.
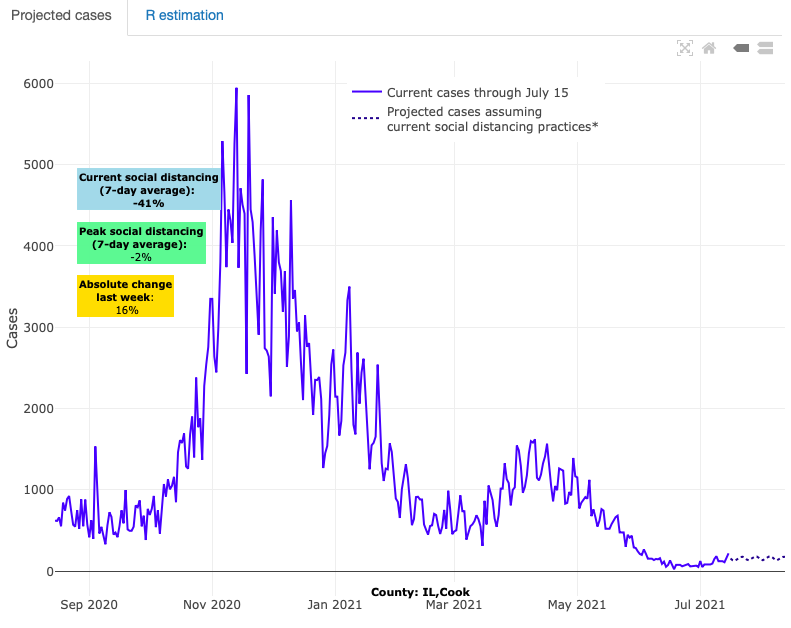
Above are the projections for Cook County (Chicago) in Illinois.
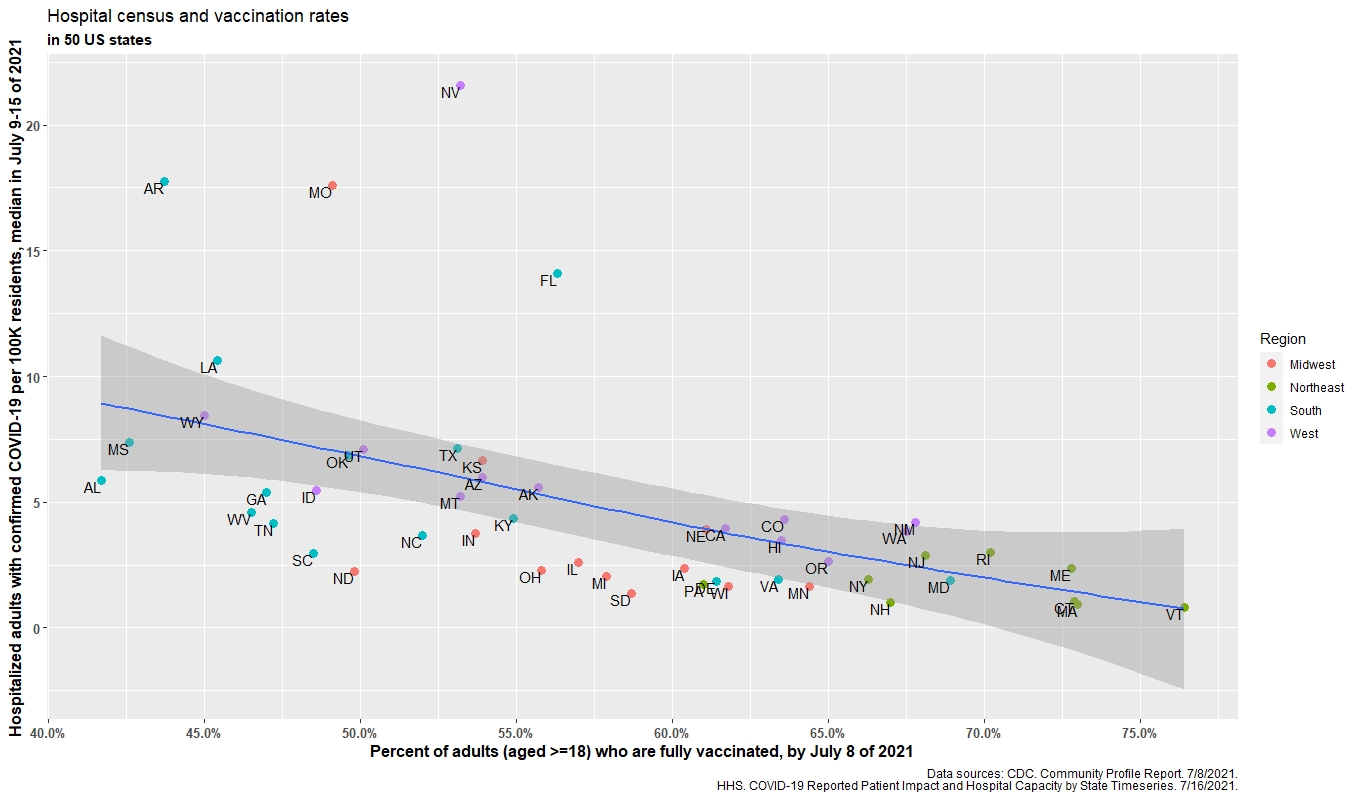
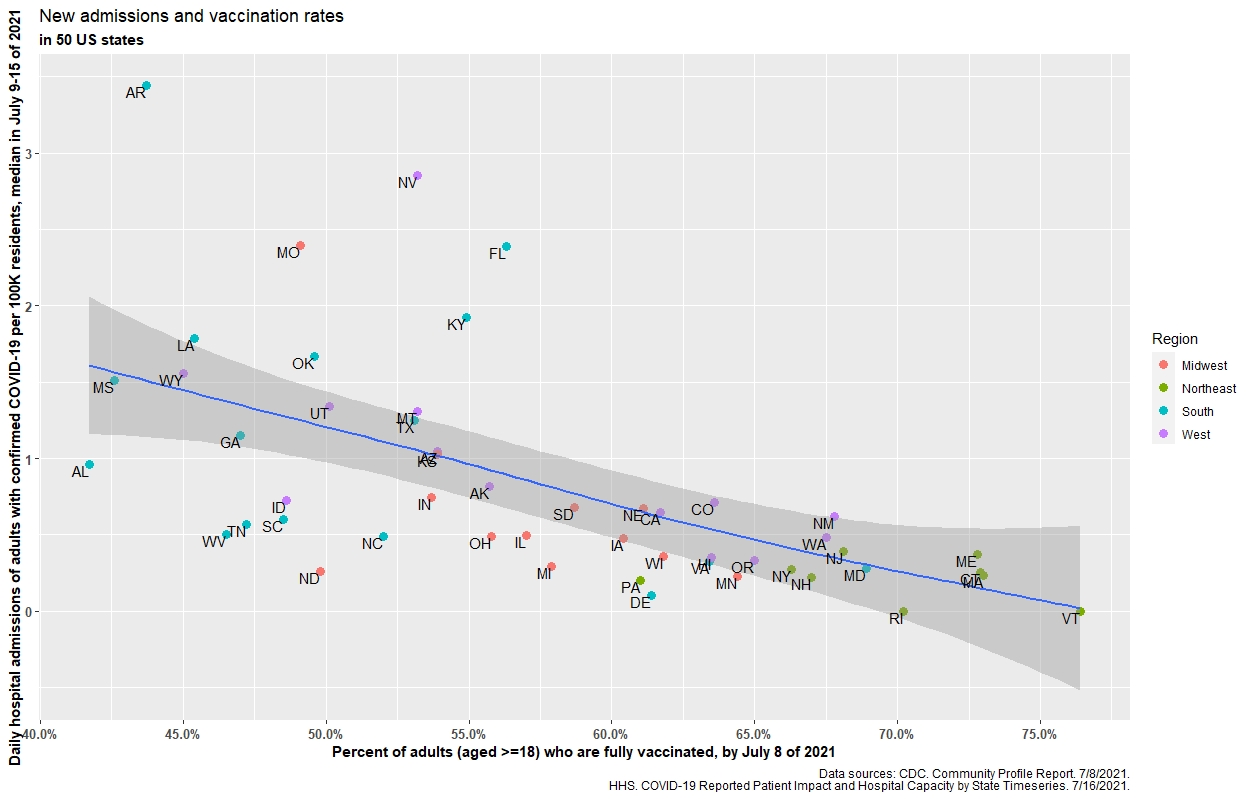
The accompanying figures give a visual display of this inverse (i.e., protective benefit) correlation between vaccination rates and hospital census, and vaccination rates and daily hospital admission by state. (Click on images to enlarge).
Hospital census and vaccination rates
Daily hospital admissions and vaccination rates
How worried should we be about the Delta Variant and recent increasing transmission across the country?
There are significant concerns regarding the emergence of the delta variant as the dominant strain in the United States. While this variant does appear to have potential for increased transmissibility, we warn against comparing current transmission rates to early periods of the pandemic when mitigation strategies were omnipresent. It is likely that some of the increased transmission attributed to the delta variant is instead a result of changes in human behavior. Regardless of the reason for the documented increase in transmission rates, we can take comfort in the fact that available vaccines are effective against these variants.
Furthermore, based on data from our models, we are hopeful that the current episodes of local resurgence will be short-lived and not nearly as widespread as they were last summer. Our models suggest that areas of Missouri and the Mountain West are nearing or already moving past their peaks after a recent significant spike in activity. Additionally, sharp inclines in local reproduction numbers experienced by many areas following the holiday have sharply declined again toward one. In prior periods of the pandemic, the regression of reproduction numbers towards one was often soon followed by a decline in incidence rates. We would expect a similar relationship during this current period. We hypothesize that this pattern of acute local spikes followed by rapid declines in reproduction numbers is the result of partial or complete protection of a given community’s populous due to vaccination and/or prior infection. Without a large pool of susceptible individuals, a resurgence will quickly peak and then subside.
However, as noted above, communities with poor vaccination rates will likely experience resurgence episodes with greater peaks and slower declines in incidence throughout the remainder of the summer and into the fall and winter seasons. It will be important to follow hospitalizations and deaths associated with these local areas of resurgence as the potential for severe disease is still real for many unvaccinated and thus vulnerable adults.
Looking ahead to fall
We will continue to follow the trends across all counties in our model as we enter into the fall and winter seasons. We anticipate that increases in incidence rates will be experienced locally in a heterogenous pattern rather than the homogeneous widespread increases that we saw across the nation last winter. As previously stated, positivity rates and transmission rates will be the indicators that signal the start of and recovery from any local resurgence.
We expect that differential weather patterns, variation in mitigation strategies, and vaccination rates will be the factors that dictate the severity and duration of resurgence that any locality might experience. Of these factors, vaccination rates are most in our control. It is our hope that this summer resurgence that appeared following our country’s reopening will persuade many individuals who have been on the fence about vaccination to quickly change their minds. Even areas that boast reasonably high vaccination rates now should not become complacent, but instead double down on their efforts to reach even higher vaccination coverage. If not, we can expect to experience larger and more sustained resurgence episodes throughout the fall and winter when weather conditions will further promote transmission.
PolicyLab’s 2021-22 K-12 school guidance has arrived
On the heels of the CDC’s long anticipated release of K-12 school guidance on July 9, PolicyLab is releasing its own updated guidance today. For the 2021-22 school year, our team has focused on helping school leaders, teachers, and families understand their options for COVID-19 prevention in schools now that emergency orders for mask use and social distancing have been eliminated in most parts of the country. Vaccination of school staff, students (currently ages 12 and above, and eventually all children), and family members is the most reliable intervention for ensuring safety during the upcoming school year and quickly returning schools to pre-pandemic activities. As some schools move toward mask-optional environments, our guidance attempts to equip schools and families with the practical advice that can help align their choices with new CDC guidance and local regulations.
We want to reassure families that we are in a different moment of the pandemic. Now that adults have been offered vaccination, the risk assessment has changed for many families and communities. This fact has led some school communities to develop more flexible mitigation strategies for the upcoming school year that aim to balance goals of limiting infection transmission and optimizing in-school learning. Some families may feel anxious about what to do for their child or children if their school reverts to a mask-optional strategy. This may be particularly acute for families with elementary-age children under 12 years of age who are not yet eligible for vaccination. We offer some guidance to these families on how to decide when to have their child mask or not mask. Families must also be aware that any school district’s recommendation for a mask-optional approach could change as COVID-19 incidence rates change throughout the fall. Some locations, especially those with poor vaccination rates, will likely have local resurgence that may lead health departments to recommend resuming masking indoors.
As we release this year’s new guidance, we hope that families, teachers and school leaders will see a pragmatic roadmap for how to navigate choices that will be individualized but dynamic in the months ahead. We are supportive of the local decisions that school districts are grappling with and recognize the need for options that reflect the compromises that families and communities are seeking as we continue to navigate the COVID-19 pandemic that persists in the United States.