COVID-19 Outlook: As Resurgence Continues, Americans Are No Longer Distancing
Last week, in our weekly blog post highlighting the main findings from our county-level COVID-Lab forecasting model, we reported that test positivity and case incidence were increasing across much of the northern United States. Now, as we emerge from the holiday week, we are bracing for the additive impact that holiday gatherings will contribute to this spring resurgence. Here is this week’s update:
- The average PCR testing positivity rate across the country increased to 6.2% in the past week (up from 5.8% last week); the majority of the 821 counties included in our model have higher testing positivity rates this week than last week.
- The average reproduction number (a measure of transmission that indicates how many additional individuals could be infected by every positive case) across the counties we follow is 1.16, which is relatively unchanged from last week. Still, 20% of these counties have a reproduction number exceeding 1.25, indicating substantial transmission.
- Regions with higher reproduction numbers and case incidence this week include the Pacific Northwest; Upper Midwest; the I-80 corridor from Illinois across Indiana, Ohio, and Pennsylvania; the I-95 corridor between Baltimore and Connecticut; and the upper reaches of New England.
- The national pediatric and adult COVID-19 hospital censuses remained flat this week, with the seven-day average for adults dropping slightly below 40,000 and pediatric census dropping below 1,000. However, some states have sustained local increases in adult hospital census: Michigan (up 200%, nearly 3,000 patients hospitalized), Pennsylvania (up 25%, nearly 2,500 hospitalized), Illinois (up 50%, nearly 1,500 hospitalized), Maryland (up 40%, nearly 1,400 hospitalized), Minnesota (up over 100%, nearly 600 hospitalized), and Washington (up 30%, nearly 500 hospitalized).
Specific areas we are monitoring:
- After a couple of weeks in which it appeared New York might stabilize, testing positivity and case incidence increased modestly last week, which led to abrupt increasing case number projections for Upstate New York and a forecast of sustained high transmission in the New York City boroughs over the next four weeks. Hospitalizations thus far have remained flat across the state.
- In the midst of climbing hospitalization rates in the Delaware Valley region of Philadelphia, southern New Jersey, and Delaware, large jumps in test positivity suggest the likelihood is increasing of additional growth in community case incidence over the next four weeks that will near winter peaks.
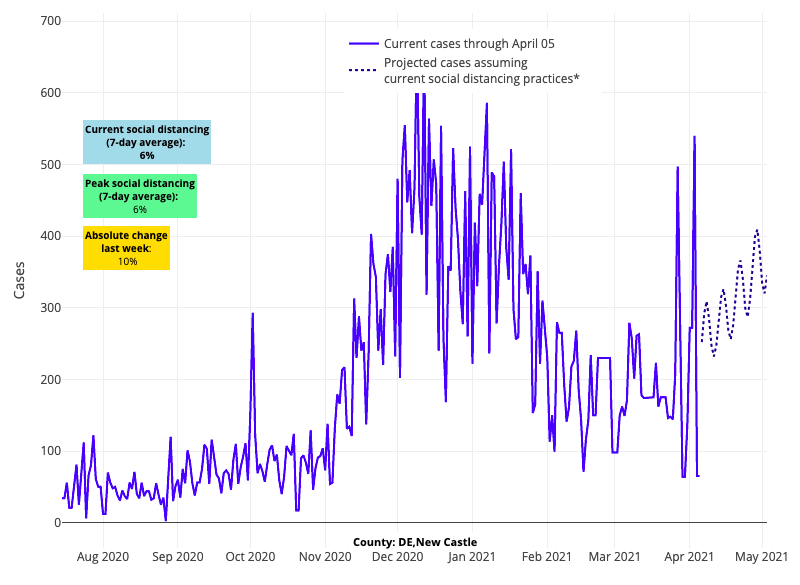
Above are the projections for New Castle County in Delaware.
- Not only has the adult hospital census surged in Michigan from 1,000 to more than 3,000 adults in the last month, but case incidence in some Michigan counties has reached or exceeded winter peaks, particularly in Macomb and St. Clair counties near Detroit.
- With increases in test positivity rates and hospitalizations across Illinois, our models project some regions of the state will experience similar transmission trends to areas of concern in Michigan. We are particularly watching Chicago and Peoria, the latter of which is experiencing community case incidence at rates similar to winter.
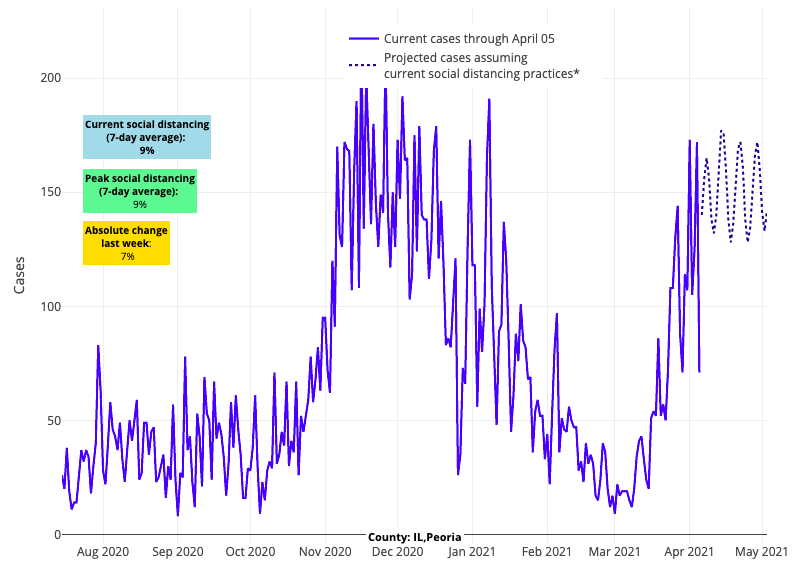
Above are the projections for Peoria County in Illinois.
- Test positivity and case incidence are increasing across Colorado again, and our models project continued growth in case incidence in many counties, including in and around Denver and Colorado Springs. For now, hospitalizations and emergency department visits have remained flat or slightly increased.
- Testing positivity rates and transmission are increasing throughout Florida, including along the southwest and southeast coasts. Interestingly, emergency department visits remain flat, and hospitalizations declined over the past week.
- There are early signs that case incidence could increase in parts of California, including the Bay Area, Sacramento and the northern Central Valley.
In this week’s data, we see case incidence increasing over a wider area of the north than last week. Michigan’s trends are particularly concerning, as it looked like the state might have hit its peak in case incidence a week ago but has now pushed beyond our projections. The continued increases in hospitalizations in Michigan should serve as a stern warning to all regions of the country, particularly those where case incidence is already on the rise.
Americans are abandoning social distancing
Much has been said about variant strains contributing to increased COVID-19 transmission throughout the country. Some reporting in the last week has suggested that the B.1.1.7 variant strain that originated in the United Kingdom has uniquely changed in its proclivity to infect younger individuals compared to earlier strains of the virus. While variants like the B.1.1.7 strain may be more transmissible, the fact is that transmission of any form of the virus relies on breeches in mitigation efforts (e.g., mask wearing and social distancing) among vulnerable individuals (i.e., those unvaccinated).
Therefore, we should not underestimate how much our collective abandonment of proven, simple mitigation strategies is contributing to the increases in case incidence and hospitalizations we are witnessing in some areas. As more individuals abandon masks while gathering with others in their homes, in restaurants, on the sidelines at youth sporting events, in and around schools, and in many other venues, we should not be surprised by the increases in case incidence.
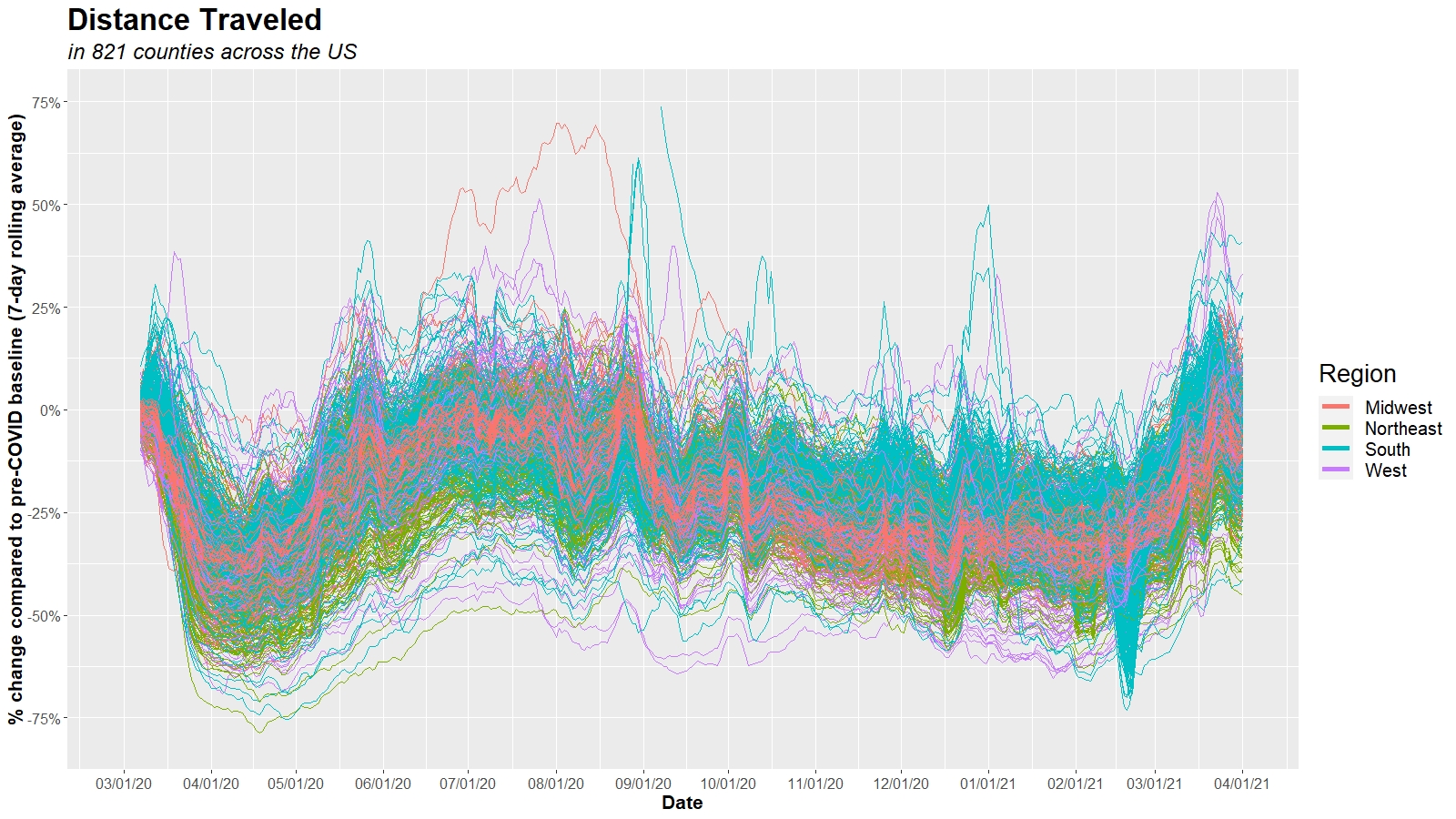
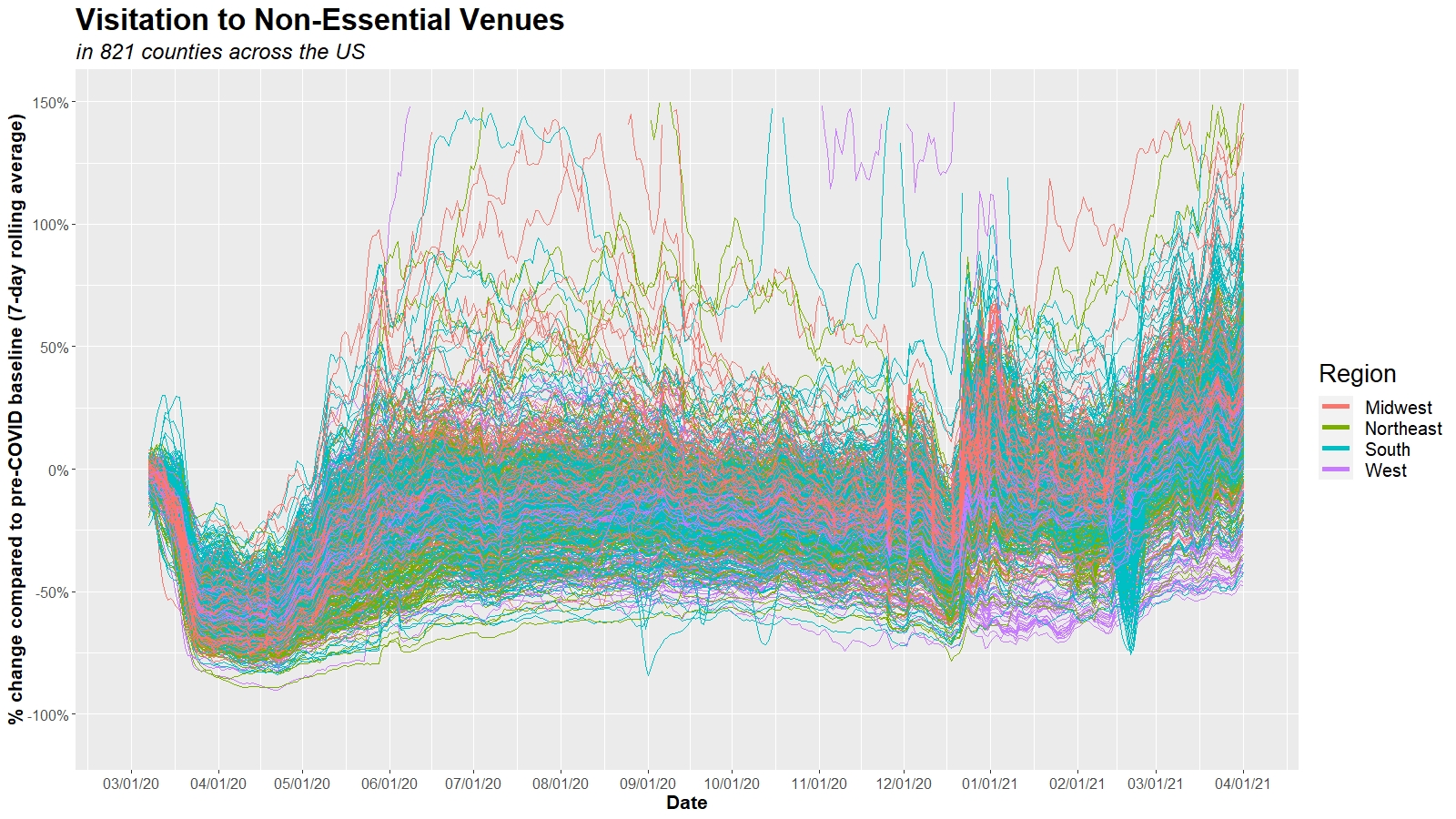
The figures below (click to enlarge) show two of the mobility variables we have been tracking throughout the pandemic. Using cellphone data from Unacast, the graphs report the total distance individuals are traveling within the 821 counties we have been following throughout the pandemic, as well as travel to nonessential businesses like retail stores and restaurants. Both are expressed as a percentage compared to pre-pandemic levels in February 2020.
While there is variation from county to county, the directionality is clear. Americans have resumed traveling and gathering, and their mobility is back to, if not exceeding, pre-pandemic levels.
Should we be concerned by increasing case incidence?
The increase in case incidence is concerning, but, as we’ve stated before, we believe that hospitalization rates are more important to track right now as they are a better marker of severe disease. As we await the impact that gatherings during spring break and recent religious holidays could have on transmission, we are concerned that if individuals do not re-embrace mask use and social distancing, hospitalizations will continue to increase across the north and begin to increase in other areas of the country.
We are especially concerned that those that have not had the opportunity to be vaccinated or have not waited long enough after vaccination to build immunity have reclaimed their social lives too quickly. By making these decisions, we are underestimating the potential of this virus to cause severe disease, even in younger adults. We appreciate pandemic fatigue, but we urge patience among all of us to allow vaccinations to catch up.
When will the pandemic end?
From the beginning, this pandemic has been defined by numbers—number of cases, number of hospitalizations, number of lives lost. A sustained, deepening spring resurgence reminds us that this pandemic persists, and we have not yet “turned the corner.” However, we can anticipate that this time will come, a time when all children will return to, and remain in, school, parents and grandparents can resume their normal lives, and young adults, well, can be young adults again.
So, how will we know when we’ve “turned the corner”? The end of this pandemic will not be marked by completely eliminating COVID-19, as we now suspect that SARS-CoV-2 is likely to become an endemic virus that peaks with seasonal transmission in the winter. Therefore, identifying arbitrary case incidence thresholds as targets may not be the ideal approach for determining the end of the pandemic. Rather our team would consider the following concepts more important:
- Offering and delivering vaccination to all adults: As the data become unequivocal that vaccination nearly extinguishes the risk for severe infection for at least six months (and likely longer), it would seem appropriate to declare the end of the pandemic once all adults who want vaccination have received it. Unfortunately, as of this week in the U.S., only 15% of individuals between 18-64 years of age have received their first vaccine dose, and only 31% had completed the full series. This is in contrast to 75% of individuals 65 and older who have received at least one dose, and a majority who are fully vaccinated. Once we’ve increased vaccination rates across all adult age groups, we will see case incidence and hospitalizations decrease throughout the country. Now is the time to clearly communicate the effectiveness and safety of these vaccines to alleviate any concerns that some may have about receiving them. It is also the time to double down on efforts to make the vaccine accessible to all individuals who want it.
- Continued circulation of SARS-CoV-2 should not deter us from claiming the end of the pandemic: We should not be surprised by seasonal resurgence of COVID-19 in the future, nor should we be surprised to see a long tail of community transmission in the coming weeks. What matters most is monitoring the burden of severe disease (as measured by hospitalizations). As vaccination rates increase hospitalizations should decline. This week, the Centers for Disease Control and Prevention released a report showing that among nearly 4,000 health care workers who were vaccinated in several regions of the country, 200 acquired COVID-19 over the ensuing three months. However, only 2 of the 200 required hospitalization. Additional studies like this will hopefully confirm that vaccination is extremely effective at reducing severe disease. When we reach a sustained period of reduced hospitalizations, that is when we can justify reducing mask use and social distancing. We foresee time-limited recommendations for masking in public locations if there is seasonal resurgence of COVID-19 alongside the flu that stretches hospital capacity, but those decisions would be made seasonally.
We must not lose hope that the end is in sight. Pundits may message that this was all caused by the variants, but that explanation neglects the more likely explanation: that many of us have moved on from the pandemic, despite it not being over yet. We still have work to do at the population and individual levels. We need to direct vaccine inventory to those areas that are still well behind in vaccination coverage. We must urge younger adult family members and friends to receive the vaccine as soon as they can, while advising them to exercise caution and patience until it is their turn. Many may have underestimated the virulence of the virus even for younger adults; rising hospitalization rates at this late stage should recalibrate those assumptions.
Individuals should know that receiving the vaccine is not just an action to end the risk for themselves, but it is also an action that serves those around them. Working to pick each other up is often referenced as the American way; we need such actions more now than ever.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia, and is a co-author of PolicyLab’s Policy Review: Evidence and Guidance for In-person Schooling during the COVID-19 Pandemic.