COVID-19 Outlook: Navigating the Final Leg of the COVID-19 Pandemic

For the last three weeks, our county-level COVID-Lab forecasting model has forecasted declining COVID-19 transmission across the country, except in some areas such as the Pacific Northwest, Colorado, Arizona and parts of the Southeast. This week, we not only see evidence of sustained improvements, but the pace of improvement is accelerating. Here are the latest updates:
- The average PCR testing positivity rate across the 821 counties included in our model remained relatively unchanged this week at 5.2%. A majority of these counties continue to have testing positivity below 5%, and only 8.6% of the counties we follow have rates above that.
- Only two states have an average testing positivity rate over 10%—Michigan, where rates have been falling relatively quickly, and South Dakota, which is the only state that had an increase of 1% or more this week.
- The average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) across the counties we follow increased from 0.92 last week to 1.03 this week; however, this appears to be driven by a subset of counties. Approximately 10% of the counties we follow are demonstrating substantial transmission with reproduction numbers over 1.25, and only 9% are seeing more than 200 weekly cases per 100,000 individuals.
Specific regional updates:
- Declines in case incidence and test positivity are particularly impressive in the New York City metropolitan region, where case incidence has fallen by 60%-80% since early April. Our models project these declines will continue.
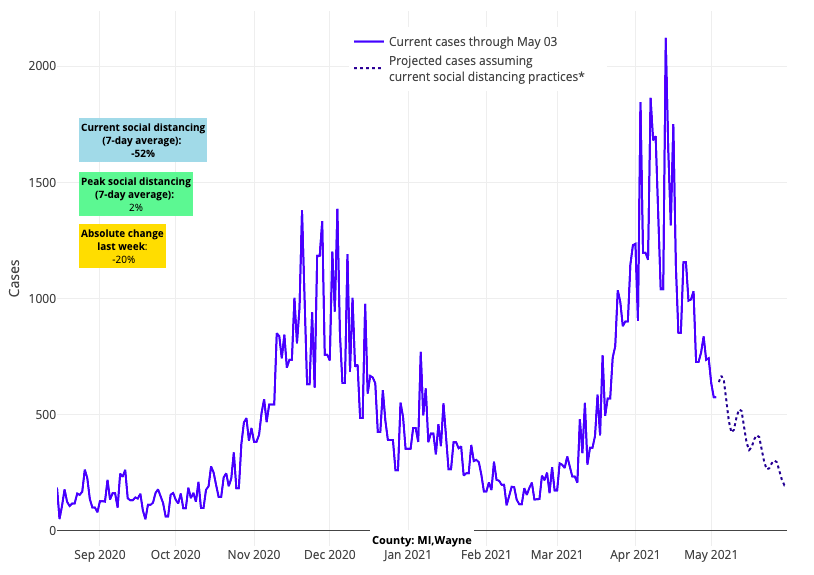
Above are the projections for Wayne County (Detroit) in Michigan.
- Michigan is another region demonstrating rapid improvement in case incidence. Our models forecast that over the next four weeks, counties in Michigan will achieve the low rates of cases they experienced in early fall 2020.
- There are some Midwestern states experiencing modest increases in test positivity and emergency department visits across multiple counties, including Indiana, Missouri, Kentucky and Kansas.
- Colorado appears to be in flux with some areas having stable or declining test positivity rates, while others have increasing transmission. For example, the Denver metropolitan area has stabilized, but test positivity rates are still increasing in Colorado Springs and Pueblo.
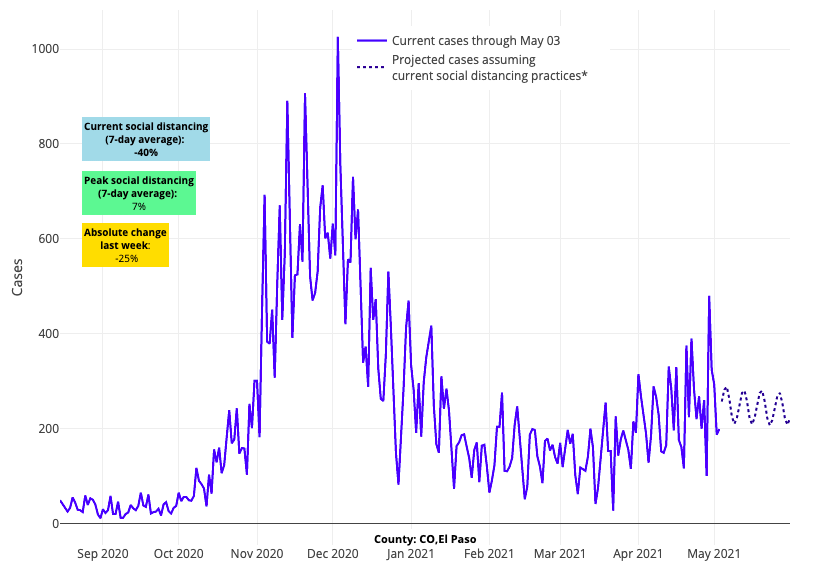
Above are the projections for El Paso County (Colorado Springs) in Colorado.
- The southern areas of the country remain stable, with Florida, Texas, Arizona, and Southern California all demonstrating flat or declining reproduction numbers.
- Reproduction numbers and test positivity rates are beginning to fall in and around Portland and Seattle, suggesting these areas are moving past their spring peaks.
Importantly, national trends in COVID-19-related hospitalizations continue to improve, even in areas experiencing increasing test positivity rates. This suggests that the proportion of cases that are more severe is decreasing.
- Nationally, adult hospital census declined further this week to about 37,000 individuals. Pediatric admissions have modestly increased in recent weeks.
- Despite persistently high emergency department visits, hospitalizations declined by half in New York (from 5,000 to 2,500) and New Jersey (from 2,500 to 1,300) in the last month.
- In Michigan, daily hospital admissions dropped by 50% within the last month. Throughout much of the rest of the Midwest, hospitalization numbers remain flat or have started to decline.
As numbers go down and population immunity increases, will herd immunity be achieved?
Much has been written this week about the unlikely possibility that “herd immunity,” and with it the elimination of SARS-CoV-2, will be reached through vaccination and/or natural infection. The inability to achieve herd immunity is multifactorial, including:
- challenges to efficiently providing vaccination to all regions of nation and the world,
- vaccine hesitancy that persists through this period,
- potential for continued emergence of variant strains, and
- uncertainty regarding the durability of immunity after natural infection or vaccination.
As we and others have said for some time, herd immunity will likely never be achieved and thus, this virus will continue to exist. While that may provoke anxiety for those who hoped for a clean ending to the COVID-19 pandemic, this does not mean that SARS-CoV-2 will persist in a pandemic state. Instead, we anticipate it will become a seasonal virus with peaks in transmission during fall and winter. Going forward, uncertainly will exist regarding how significant yearly peaks will be and what proportion of those seasonal cases will be severe.
As numbers decline, do I really need to be vaccinated?
Much of what happens in the future may likely depend on how many of us get vaccinated in the coming months. As case incidence continues to decline throughout the country, it is likely that some individuals will become reticent or more complacent about vaccination. Some that received their first dose may be less motivated to return for their second and others may decide their risk is low and not get vaccinated at all.
We also recognize that some with a history of prior infection may conclude they do not require vaccination because they have natural immunity against future infection. It is true that natural infection will provide some degree of protection against future infection. Israel, for example, initially prioritized who received vaccination based on data that natural infection protected individuals for several months. But we would caution that the durability of immunity from natural infection is not well defined. While additional investigation is needed, early data suggest that immunity after vaccination is more robust and may be present for longer periods of time. As there have been no safety concerns identified among individuals vaccinated after prior infection, the balance of the data would favor vaccination of all individuals regardless of prior infection status.
How will we know when we have reached the end of this pandemic?
People awaiting a proclamation anytime soon that the pandemic has ended are likely to be disappointed. A long tail of declining transmission with occasional regional resurgence will make such endpoints difficult to declare. That said, we are likely to return to mostly normal this summer as overall rates of transmission continue to fall, and as vaccination coverage increases across the country. Even with the potential for increased cases in the fall and winter due to seasonal transmission, we will continue our path to normalcy. Humans have existed through centuries of respiratory viral seasons—we will have to learn how to co-exist with SARS-CoV-2 as well.
In the meantime, achieving continued success with vaccinations will serve to keep incidence low through the summer and blunt the potential for substantial resurgence next fall. Unfortunately, despite significant early demand for vaccines, vaccination rates have now plateaued near 60%. Novel approaches are needed to optimize vaccination rates. This includes facilitating easy access of vaccinations to all individuals. The focus should transition from large vaccination centers to local vaccine clinics that target areas with poor existing coverage. There are other methods to consider as well, such as behavioral economic techniques being used in Israel. Israelis who are vaccinated can move with much greater freedom across the country, providing a clear incentive for vaccination. Just recently, the University of Notre Dame challenged its students to reach high levels of vaccination coverage on campus in exchange more quickly removing restrictions and masking—and the students succeeded in reaching the goal.
For many, this may feel like an uncertain time in which public health guidance is confusing and endpoints are difficult to pinpoint. As neighbors and families see the benefits of vaccination, we suspect and have seen that many who waited out the first round may now seek their turn in line. New York and the greater Northeast demonstrated in the last couple of weeks that achieving high rates of vaccination quickly can quicken the pace toward a strong recovery. As vaccinations build in other regions, we would expect similar turning points. It’s time to close out the final leg of the COVID-19 pandemic.
