COVID-19 Outlook: The Fall Wave is Here, but its Outcome is Not Predetermined
This week, PolicyLab released a long-awaited and important update to our guidance for schools during the pandemic. So much has changed in the eight weeks since we first posted our guidance back in August. We’ve seen schools open throughout the country with varying approaches, amidst differential community incidence rates and leveraging variable safety plans. Youth extracurricular activities have also resumed with similar variance. Simultaneously, in our COVID-Lab data, we’ve seen a large fall wave grip the country, beginning in the Midwest and Mountain States and now spreading east, west and, increasingly, south.
The reassuring news is that returning children to school has infrequently been a driver of community transmission and, when it has occurred, it has principally been in areas with very high transmission rates and in the absence of strong safety protocols. Still, the many schools that continue to do well with in-person learning and are likely not currently contributing to community transmission should recognize that if their area starts to see sustained significant rises in case counts, it will threaten their ability to preserve the safety of in-person schooling. This is the major challenge that we will grapple with in the coming weeks.
During this dynamic period of continuous change in incidence, weather, and school safety plans, we find ourselves in the midst of a natural experiment. We are learning on an almost daily basis about the strengths—and sometimes weaknesses—of our mitigation strategies, in particular plans to protect schools from experiencing transmission within their walls. The foundation of the safety plans remain the same—mask wearing, social distancing, staying home when symptomatic and hand hygiene. As case incidence increases in schools’ communities, a commitment to contact tracing specific to in-school transmission will also become paramount, which some schools have already recognized. We are witnessing in real time the success of school systems that have been able to commit to these tenants of mitigation. Whether they can stand up to higher community incidence rates still remains to be seen, and this we need to watch closely each week.
The changes in the PolicyLab guidance released today are reflective of all that we are learning. Our new guidance has moved away from the absolution of testing positivity or case incidence thresholds to an increasing reliance on the collaborative decision-making with health departments that are meticulously doing the contact tracing when students and teachers acquire COVID-19. (We applaud all of our colleagues in public health; their efforts are herculean in nature and are often under-appreciated.) We have more precise guidance for mitigating risk during extracurricular events such as youth sports, music practices and theater activities. We also provide a menu of questions that school leaders can ask, alongside their local health departments, as they navigate the months ahead—months that we know will be fraught with challenging decisions.
Some highlights of the updated document include:
- Multi-layered strategies work to reduce transmission risk during the school day. We have added important details to illustrate how these layers are necessary to protect students and staff. In the context of “pandemic fatigue,” we urge school communities to maintain energy and commitment to the implementation of safety plans and draw motivation from emerging data on their effectiveness.
- As noted above, the guidance has shifted away from a dependence on community thresholds of incidence and case positivity. Instead, schools need to focus on monitoring for and preventing linked transmission among students and teachers during the school day. Additionally, we need to continue to stress the importance of maintaining mitigation strategies beyond the school grounds, such as during carpools and after-school activities. Parents can assist by avoiding sleepovers and large weekend parties with students.
- We are learning that most transmission in youth sports leagues is occurring off the field; in locker rooms, pre-game meetings or meals; or during transportation to and from the games. Maintaining social distancing and mask wearing in these off-field activities will preserve the ability to continue on-field activities. This includes parents attending these events—wear your masks and social distance.
- We are learning of the necessity of contact tracing and testing, especially as we enter a period of increasing transmission, to inform decisions of when to revert to distance learning and, worse yet, when to close schools because of developing outbreaks.
Turning back to PolicyLab’s COVID-Lab forecasts, we see the challenges very clearly. The fall wave continues to grip most of the country. The forecasts across the Midwest show no sign of abating. Wisconsin leads the way with another week of increasing test positivity rates and exponential growth in cases. Concerningly, this growth is now projected to spread across Illinois, Indiana, Michigan, Ohio, Nebraska, Minnesota, the Dakotas and the Mountain States threatening major cities like Chicago, Indianapolis and Denver.
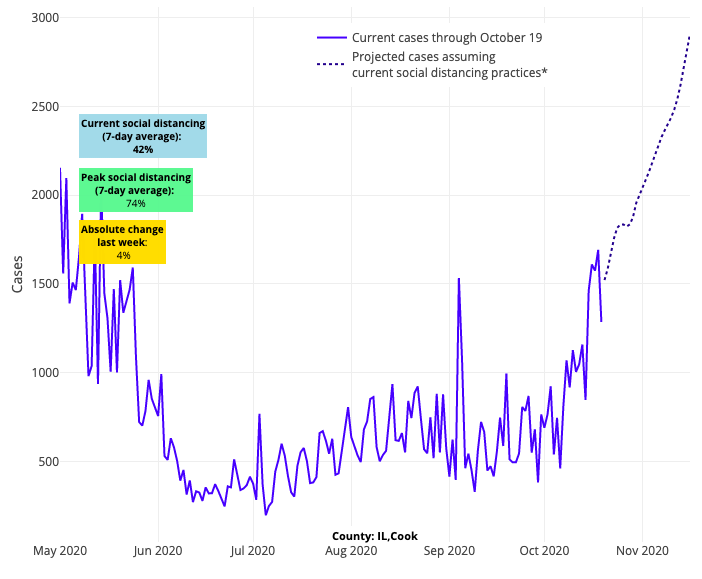
Above are the projections for Cook County (Chicago) in Illinois.
But, it is not only the Midwest that is troubling; we are also seeing worsening forecasts for metropolitan areas in Tennessee and Arizona, as well as Dallas and other parts of northern Texas.
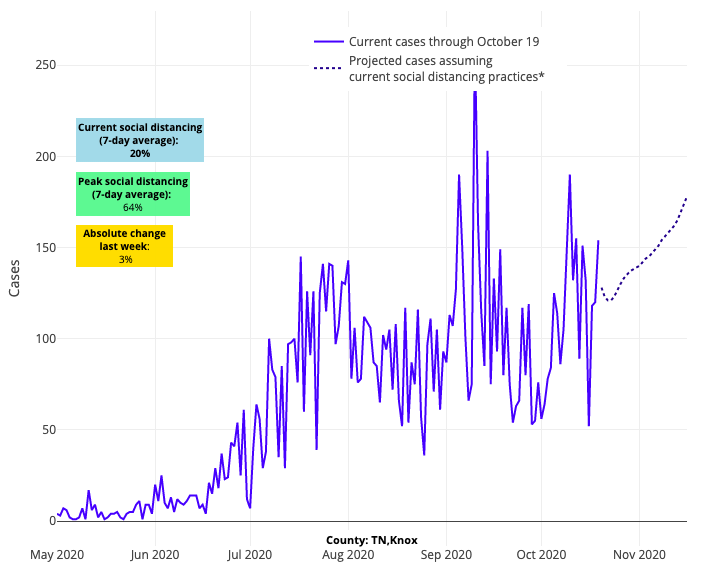
Above are the projections for Knox County in Tennessee.
At the same time, we find solace in the success of the many states across the Pacific Northwest and Northeast that continue to thwart exponential growth in COVID-19 incidence. Our forecasts for Oregon suggest a slowing in the amplitude of growth again this week. Massachusetts and New York do have increased incidence rates, but at a much slower pace than the rest of the region.
When it comes to New York, we hypothesize that these slowed outbreaks are the result of quick, early actions by leaders to address any emerging hotspots. Also encouraging this week in New York City, is the revelation that COVID-19 infection has largely been prevented among students and teachers during the early weeks of school reopening. This is directly attributable to the considerable preparations put in place in advance of opening. However, we do caution citizens of Manhattan and Staten Island, where new risk may be emerging (see below); stay committed to your mask wearing and social distancing protocols.
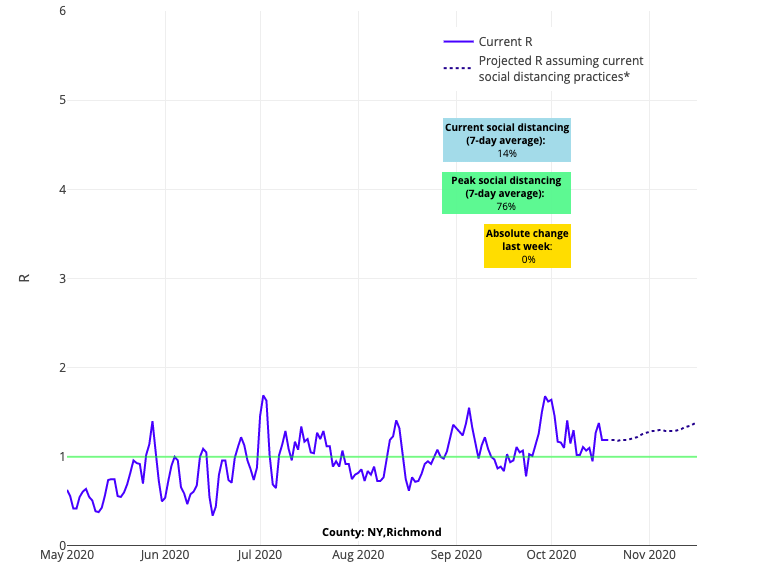
Above is the R graph for Richmond County (Staten Island) in New York.
These signs for optimism, however, are tempered by happenings in other regions of the Northeast. Projected case counts in the large, populated areas of northern New Jersey have begun to accelerate in our forecasts, and we are seeing soaring test positivity and case incidence in many areas of Pennsylvania, excepting Philadelphia, which has thus far weathered the storm.
Finally, even as our projections for Florida, Louisiana, and California remain stable comparatively to other areas of the country, we are just seeing communities in these states move past their nadir and are now at risk for significant case count increases in the coming weeks. This includes Sacramento, the Bay Area, and Florida’s Miami and Broward Counties. That said, these regions should not throw up their hands and accept this projected fate. As we have seen in other areas of the country, rising incidence rates can be stymied with a collective community commitment to safety protocols.
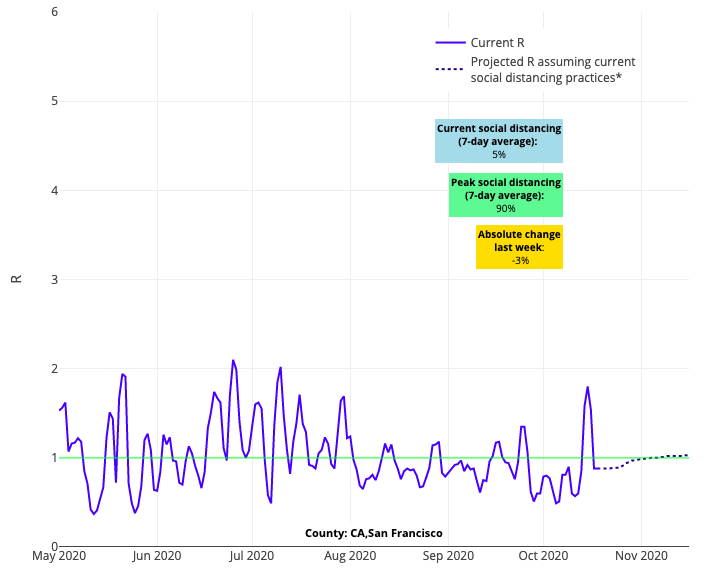
Above is the R graph for San Francisco County in California.
Rising caseloads need to also be interpreted alongside hospitalization rates. Of concern, is that more than 80% of states have had increasing COVID-related hospitalizations in the last month, and 12 of the 18 states reporting pediatric COVID-19 hospitalizations to the U.S. Department of Health and Human Services are showing increasing trends, albeit at low numbers. This bears close watching; if hospitalizations can stabilize through local vigilance and focused interventions by state and county leaders, we may yet traverse the remainder of the year without significant restrictions.
Right now, we would emphasize that much uncertainty remains, even as this wave persists. Interestingly, 12 of the states with rising hospitalizations reached a plateau of hospital census this past week, despite continued case growth. Further, many states have relatively low numbers of ICU stays even after hospitalizations had increased in prior weeks. We are not quite sure why this last point is true, but will offer a few possibilities:
- We may have improved our ability to protect the most vulnerable individuals, such that those who become sick and require hospitalization are younger and/or at baseline are healthier and thus are able to recover.
- We are better at treating COVID-19, meaning fewer patients need ICU care.
- In this period of the pandemic, there may be reduced inoculums of virus exposure in those that are being infected. This could be a result of mask use and distancing that serve to blunt the degree of exposure.
Fortunately, the number of deaths have not yet increased at a rate that is commiserate with rising incidence. Similar explanations for stable hospitalization rates in certain regions might also explain why we are not yet seeing case fatality rates rise to the levels we saw early in the pandemic. However, we must maintain caution when considering these trends, as while deaths are not yet increasing they are persisting, with many individuals dying from COVID-19 each day. And it may be that we are too early to see the growth in fatalities that could befall the country. Most public health experts suspect that it is just a matter of time.
We’ve intentionally tried not to be too speculative in which way this will break in the coming weeks, even despite overwhelming evidence that a wave of infection, potentially of greater magnitude than the spring, has begun. This journey has never been linear, and we are likely to have fits and starts within and across regions. Regardless of what is to come we should not underestimate our role as individual citizens to respond to these changes. A collective and reflexive response among us to grab that mask again and reduce the size of our gatherings is perhaps our best defense. The road may be bumpy, but perhaps we can preserve in-person school, avoid our hospitals over-filling, and protect our vulnerable family members and relatives. The outcomes may feel inevitable, but they are not—they are within our control.
Gregory Tasian, MD, MSc, MSCE, is an associate professor of urology and epidemiology and a senior scholar in the Center for Clinical Epidemiology and Biostatistics at the University of Pennsylvania Perelman School of Medicine. He is also an attending pediatric urologist in the Division of Urology at Children's Hospital of Philadelphia.
