COVID-19 Outlook: A Fall Resurgence of Uncertain Magnitude Develops as We Await Vaccines for Children

With uncertainty about the trajectory of the pandemic as the weather grows colder and the winter holidays approach, we’re continuing our weekly COVID-Lab modeling updates so communities have local data at their fingertips. Let’s start with an overview of the national data:
- The average PCR test positivity rate across the 813 U.S. counties included in our model declined to 9.2%, down from 9.8% last week. Still, one-third of these counties saw test positivity rates increase in the last week. States with the greatest absolute increases in test positivity include (in order of highest to lowest): Montana, Alaska, New Mexico, Minnesota, Colorado, New Hampshire, Vermont, Utah, Wisconsin and South Dakota.
- Average reproduction numbers (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) remained around 0.9 this week, but most counties we’re monitoring are experiencing an increase in their reproduction numbers—one-quarter reached above 1, indicating growing transmission. Counties with reproduction numbers above 1 are concentrated in the Upper Midwest, Mountain States, Pacific Northwest and Desert Southwest.
- The nation’s average case incidence remains elevated at 250 weekly cases per 100,000 residents; most counties we’re monitoring are reporting more than 200 weekly cases per 100,000 residents.
- National COVID-19-related hospitalizations continued to decline this week to 50,000 adults and 800 children. Declines in hospitalizations were most pronounced in the Southeast, Mid-Atlantic and California. However, hospitalizations are increasing again in the Upper Midwest and Mountain States.
Here are some updates on the states/regions we are more closely monitoring:
- In Montana, cities are experiencing the highest rates of case incidence and hospitalizations they have seen throughout the pandemic, mirroring what happened in Idaho just a couple of weeks ago. Our forecasts continue to worsen for Utah, specifically the Salt Lake City region, as resurgence spreads to a wider geographic area.
- In the Midwest, many counties throughout Minnesota and Michigan have had a significant resurgence in case incidence, which we project will continue over the next four weeks. While we’re forecasting that case incidence will remain flat in Chicago (Cook County) into November, reproduction numbers throughout Illinois are now climbing above 1, which will bear watching.
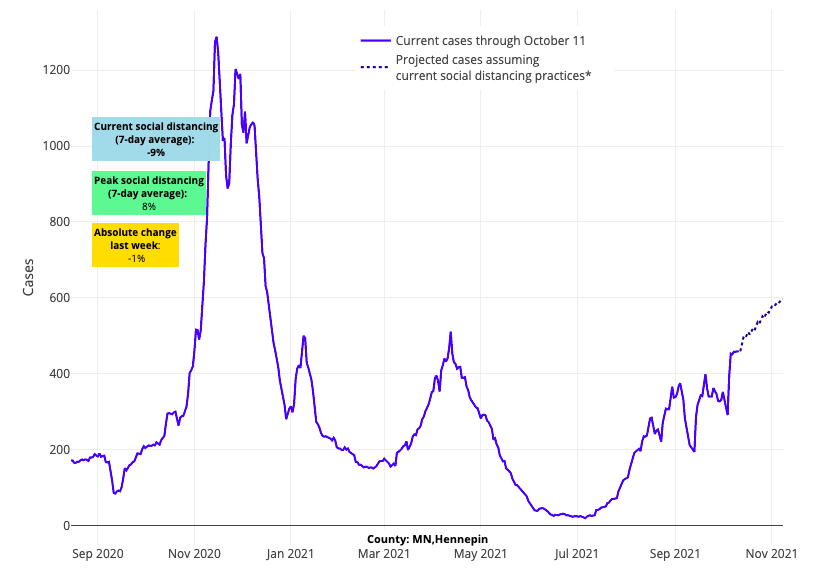
Above are the projections for Hennepin County in Minnesota.
- Test positivity rates are increasing again in Washington state, and our models project continued growth in case incidence over the next four weeks.
- Concerns we raised last week about New Mexico are substantiated in this week’s data. Our projections show case incidence will continue to grow across the state in the coming weeks. Similar increases are now extending into western New Mexico and Arizona.
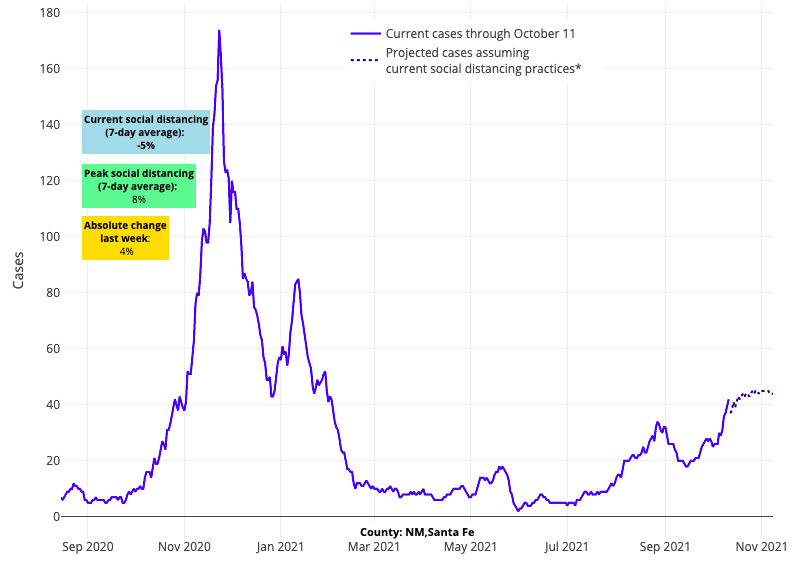
Above are the projections for Santa Fe County in New Mexico.
- California’s cities continue their slow improvement, with our forecasts showing declining case incidence in places like Los Angeles for the next four weeks.
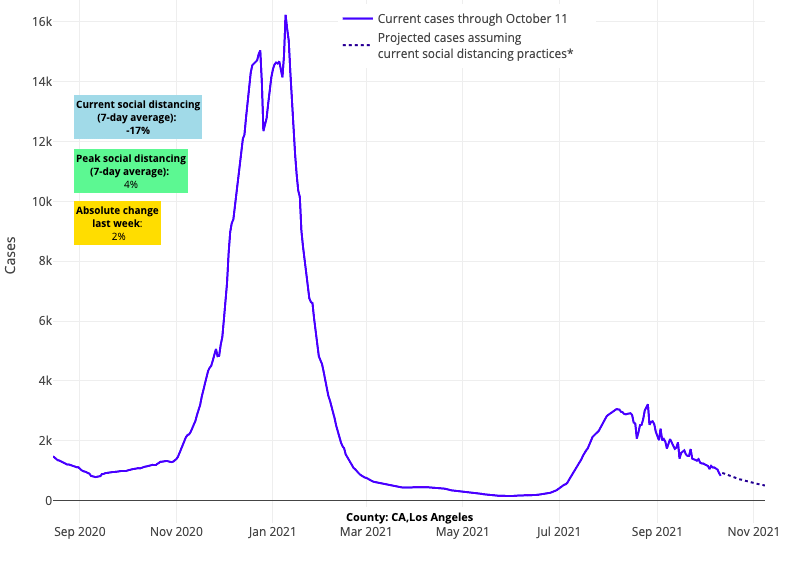
Above are the projections for Los Angeles County in California.
- While Maine and New Hampshire continue to struggle with high case incidence, the rest of the Northeast is experiencing flat case incidence, which we forecast will continue, or even modestly decline, through the end of the month.
- Case incidence continues to swiftly decline in the Southeast and lower Midwest, although at a slower rate than in previous weeks.
The Upper Midwest Has Another Difficult Week
We can take some comfort this week in the fact that national daily case counts have dropped below 100,000 and national adult and pediatric hospital censuses have declined by 50% since late summer (to 50,000 and 800 individuals, respectively). However, as has been the case, we must remain cognizant of the regional differences in case incidence and risk for resurgence.
Our models now forecast, even with declining transmission in the Southeast and Mid-Atlantic and in California, that a period of resurgence is developing for northern regions of the country.
Local increases in case incidence are being accompanied by an uptick in hospitalizations. As declining incidence begins to slow in regions that are improving, national case incidence is likely to hit a low for the fall in the next couple of weeks before increasing again. Minnesota’s adult hospital census is up over 30% since early September, and pediatric hospital census has increased from 10 to 30 children. Over the same time period, Michigan experienced a 10-fold increase in adult hospital census to 2,000 patients and a doubling of its pediatric hospital census to 40 children.
These data suggest that further optimization of vaccination coverage (beyond the 60% and 70% of adults that have received at least one vaccine dose in Michigan and Minnesota, respectively) will likely be necessary to suppress climbing hospitalizations in these states during the upcoming holiday season. The current experience in Illinois—where more than 80% of adults have received at least one vaccine dose and hospitalization rates remain flat—supports this idea.
The regional variation across the country makes predicting the trajectory of this period of the pandemic challenging. While the likelihood of a fall/winter resurgence in northern areas seems more probable this week, there is uncertainty about the magnitude, duration and breadth of geographic regions that will be impacted. Alaska, for example, which had a very difficult early fall, saw declining hospital admissions this week and appears to be moving past a peak in its adult hospital census. In the Northeast, the late summer and early fall have been relatively stable, but now some parts of this region are experiencing a bump in case incidence and emergency department visits. We need to expect that, as we enter a season of shorter, colder days that will push more people to gather indoors, we will soon see a widening geographic distribution of resurgent transmission in many locations.
Vaccinations for Children are Coming
The Food and Drug Administration (FDA) is reviewing data this week that may lead to a recommendation for adult booster doses of the Moderna and Johnson & Johnson vaccines. We are also eagerly awaiting the FDA meetings on vaccinations for children 5 to 11 years of age later this month. Certainly, it is welcome news that this meeting will take place. However, we cannot help but wonder how impactful an earlier meeting to review the pediatric data could have been. The sooner we include children among the vaccinated, the safer the latter half of our fall and winter season will be.
This leads us to address a debate increasingly being played out in the media regarding differing opinions about vaccinating our younger children. Those against vaccinating younger children support their position with the fact that children are at lower risk of severe disease from COVID-19. While we agree that the risks of severe disease from COVID-19 have been lower in children compared to adults throughout the pandemic, we would remind our readers that that risk is not zero. Nearly 700 children in the U.S. have died thus far from COVID-19, a number that exceeds mortality rates from other diseases with mandated childhood vaccines.
We also need to be aware that there are significant benefits to vaccinating children beyond just preventing severe disease or death. First, preventing SARS-CoV-2 infection may alleviate the risk of secondary complications from COVID-19 that we are just beginning to identify. For example, endocrinologists have discovered an association between COVID-19 infection and Type 1 diabetes that is being further investigated. Second, we know that even mild respiratory infections can result in significant increases in school absenteeism. Children have already missed too much school during this pandemic, and vaccination has the potential to preserve in-school learning that might be lost by COVID-19 illnesses.
Finally, no child lives in a bubble; they are active members of our communities. Each has caregivers and grandparents. Each has teachers, coaches, and adult mentors within their own families. The data on vaccinations reducing overall community spread, hospitalizations and mortality is indisputable. While vaccines are not impenetrable to some breakthrough infections, at very high vaccination rates the virus has a more difficult time propagating and is more quickly extinguished. We must recognize as a country that a 56% vaccination rate (inclusive of children) is insufficient to protect regions from the recurrent COVID-19 waves that we are seeing. Returning our communities and schools more quickly to a normal footing, where COVID-19 becomes an endemic background infection, rests on the participation of children in community vaccination campaigns.
The disruption to the social-emotional, educational and physical health of our children caused by this pandemic is unprecedented. Vaccination is, by far, the most effective mitigation strategy to reverse this.
For these reasons, we support vaccinating children once approvals are granted. It’s important to note that for each pediatric age group, starting with those 5-11 years old, COVID-19 vaccines will undergo rigorous safety testing before approval. Our team looks forward to November when children can join this collective effort, reducing anxiety within their own families and across their communities—and ushering us toward the last phase of this pandemic.
Jeffrey Gerber, MD, PhD, is associate chief clinical research officer of Children’s Hospital of Philadelphia's Research Institute.
