Learning from Innovation: Supporting Families Impacted by Opioid Use Disorder through Evidence-based Home Visiting
With more than 8 million children in the U.S. living with a parent with opioid use disorder (OUD), systems of care to promote stability and well-being for families impacted by substance use disorder (SUD) are a public health priority. The substance use crisis has corresponded with more families having more touchpoints with the child welfare system. In fact, the prevalence of parental substance abuse as an identified condition of placement in out-of-home care has increased more than 20% since 2000, and half of the children under age 1 removed from their homes in 2019 had parental substance abuse as an identified condition of removal.
While evidence-based maternal and child home visiting programs have a long history of serving families with OUD, these programs have relied on internally focused changes, such as staff trainings, and have struggled to see improvements in staff comfort or established referral pathways to more targeted SUD support services.
Seeing a chance for innovation, the Pennsylvania Office of Child Development and Early Learning (OCDEL) created an opportunity in 2018 to test new care models through home visiting programs to better address the needs of families with young children impacted by substance use. OCDEL invited evidence-based home visiting programs to submit their best ideas based on their local community needs and existing services, ultimately selecting 20 sites to pilot their novel programs.
Knowing that there was a lot to learn from sites’ implementation experiences that could be shared with other agencies aiming to engage and support families and young children impacted by OUD, OCDEL paired this pilot with an evaluation. PolicyLab was fortunate to be selected as an evaluation partner for this work. Together, OCDEL and PolicyLab designed an implementation evaluation of pilot efforts that provided staff insight into the impact new engagement strategies had on families and identified facilitators and barriers to practice change.
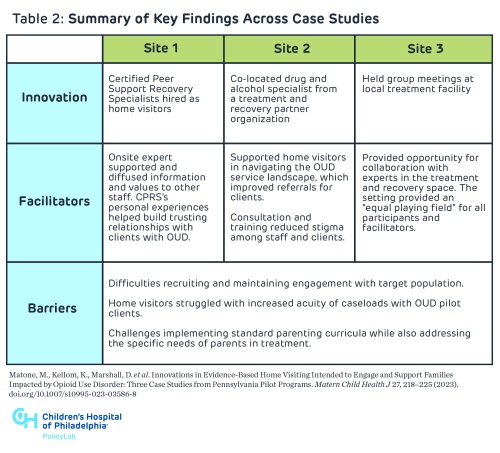
To highlight the most promising practices and lessons learned from this work, the evaluation team identified three pilot sites to conduct case studies on to provide rich, context-specific details transferable to services striving to support parents with OUD. The following chart outlines our findings, originally published in the Maternal Child Health Journal:
We learned that there are tangible opportunities for these parenting-focused services to infuse OUD expertise into their models, improve staff comfort related to partnering with parents with OUD, and better integrate services across systems to improve family engagement and meet them “where they are.” Among the promising practice innovations the evaluation identified were staffing models that included peer support recovery specialists, colocation of home visiting staff with drug and alcohol county agencies and holding parenting groups at treatment facilities.
The pilot sites learned several lessons and generated ideas for the field to carry forward and continue testing, including the importance of reduced staffing ratios among home visitors serving families impacted by OUD, recruitment and engagement strategies for families impacted by OUD navigating multiple systems, and the use of OUD- and trauma-informed models of delivering programming.
Given the widespread expansion of home visiting programs in the last decade, it’s necessary that we continue identifying opportunities and evaluating the impact these services can have on families impacted by OUD and, broadly, on family stability and maternal and child health outcomes.