COVID-19 Outlook: Preparing for Spring

Here are the overall findings from this week’s update to our COVID-Lab forecasting model:
- For the second week in a row, nearly all states experienced a decline in test positivity, with the average rate falling to 11% across the 823 counties we follow in our model. Only 18% of these counties saw an increase in their testing positivity rate in the last week.
- About 90% of the counties we follow in our model are seeing reproduction numbers below 1, indicating declining case transmission across the country. This includes California, though many areas throughout the state continue to see high testing positivity rates. Los Angeles County is the outlier as they continue to average over 10,000 cases a day, indicating that substantial transmission persists.
- While most large cities continue to see declining risk for resurgence in our models, in New York City reproduction numbers remain above 1, test positivity has still not crested in the Bronx or Queens, and their projections predict sustained peak transmission in the coming weeks.
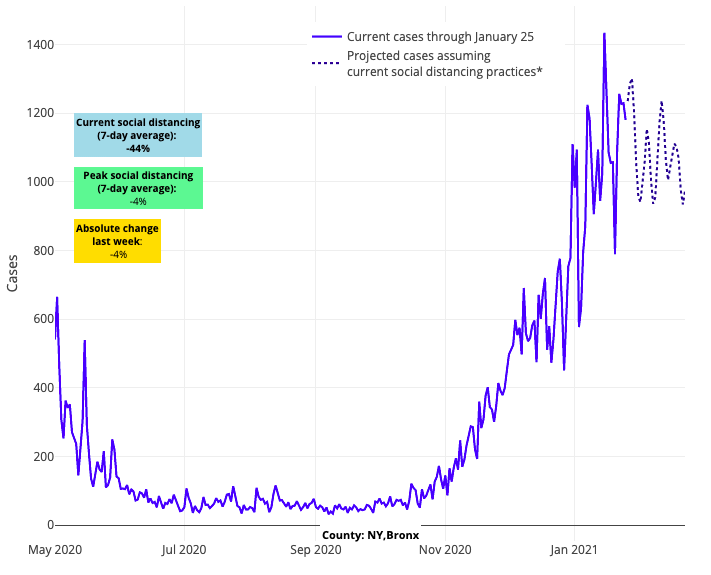
Above are the projections for Bronx County in New York.
- Our projections show areas around Washington, D.C. will continue to stall at peak transmission over the next four weeks.
- In the Southeast, forecasts have improved for the Carolinas, but Florida’s projections remain concerning. We are forecasting that communities across the state will continue to see substantial transmission through February. For example, our projections show Miami will continue to see nearly 600 weekly cases per 100,000 residents for the next four weeks.
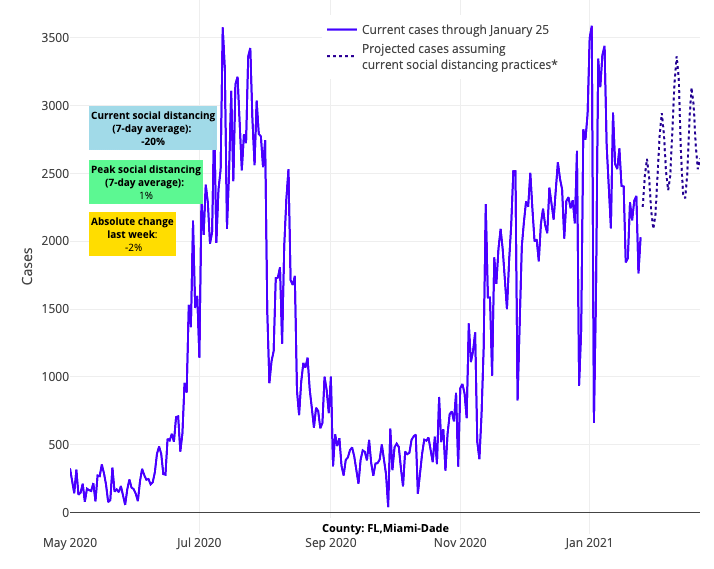
Above are the projections for Miami-Dade County in Florida.
- As deaths in Texas continue to peak at around 250 per day, we project counties in both north and south Texas will sustain high case counts in the coming weeks, although a decline in testing positivity throughout the state may suggest they are moving past peak hospitalizations and cases.
Over the last couple of weeks, our team has been encouraged to see many regions across the United States cresting the peaks of their winter holiday surges in case incidence, hospitalizations and mortality. Acknowledging that the pandemic has taught us that nothing is guaranteed, we do feel a sense of growing optimism. Our projections in most regions of the country suggest that we will see an overall decline in test positivity rates and case incidence over the next four weeks, and in areas that are not yet at their projected peak in case incidence—namely the Northeast, Mid-Atlantic, Southeast and Texas—declines in test positivity and hospitalization rates suggest things will improve there soon too. We are hopeful that a national commitment to mask wearing, increases in vaccination rates, and warmer weather on the horizon will allow for a sustained decline in rates of COVID-19 infections for the months to come.
However, the threat remains for potential increases in transmission due to COVID-19 variants emerging around the world. If variant strains are to add risk in the coming weeks, we suspect we might see it first in the New York City region. Not only does New York City see travel from countries where these variant strains were identified, but the British variant has already been reported in this area, and their continued growth in both hospitalizations and case incidence stands out as an outlier in the data from the last few weeks. We will be watching this area, and the Mid-Atlantic, closely in the coming weeks to see if another resurgence is still possible, or whether they, too, will begin to see improving projections.
With this backdrop, many schools and families are asking how these trends might influence school planning for the remainder of the academic year.
PolicyLab hosted a virtual conversation last week, titled “From Testing to Vaccines to Equity: Navigating the Remainder of the COVID-19 School Year,” to both provide answers to this question and help school communities prepare for a safe return to in-person during the next few months. We were fortunate to have the wisdom of our infectious disease partners Drs. Paul Offit and Susan Coffin to review the value of vaccines and assurance testing. These measures alongside other mitigation strategies, such as mask wearing, will increase the safety of the school environment this spring.
Commissioner Angélica Infante-Green, from Rhode Island’s Department of Education, joined us to discuss how multi-layered safety protocols have allowed schools in her state to retain safety while reopening more fully than schools in most other parts of the country. Ms. Barbara Bungy from Education Plus Health in Philadelphia, spoke of the critical role of school nurses and the need to engage communities disproportionately impacted by the pandemic proactively in planning for school reopening in the coming months. Finally, Dr. Sindhu Srinivas, the director of obstetrical services at the Hospital of the University of Pennsylvania, provided important guidance on the COVID-19 vaccine for pregnant and lactating mothers, which should be helpful for young families whose children go to school, as well as expecting parents who are among our school staff.
What Changes in Vaccine Prioritization Means for Schools
Our virtual conversation also focused on the challenges faced by many schools that are planning for when, and how, to return more children to the classroom. Certainly, those decisions were challenged this past week as we learned about shortages of vaccine inventory, continued distribution challenges at the local level, and federal changes in vaccine prioritization—which collectively suggest that many teachers may not receive the vaccine until later in the spring.
While these factors are extremely disappointing, we recognize that many communities were already preparing for a several-month process to vaccinate all school staff, given the need to split limited allocations of vaccine across several priority populations. Therefore, vaccination roll out and return to school efforts were always going to be done in parallel.
We are still confident that even in the face of these vaccine delays it is appropriate to move forward with more in-person schooling, leveraging multilayered safety protocols. Our observations of the successes many schools have had with in-person learning—even during the height of the pandemic—reinforces our knowledge that these multilayered safety plans can and will provide substantial protection for our school staff and students. For more on the evidence behind different school-based mitigation efforts and our guidance on in-school operations during the pandemic, see our policy review. A recent publication from the Centers for Disease Control and Prevention provides additional reassuring perspective that these protocols have proven their worth in school settings throughout the fall and winter.
As we support a return to in-person schooling, we will continue to advocate for more efficient vaccine roll out to school staff. A couple of weeks ago, our team discussed a strategy for prioritizing vaccination among school staff. We advised schools to consider occupational risk exposure and personal staff risk. As our public health departments pivoted to prioritizing the vaccination of older individuals and working age-adults with chronic conditions before more broadly immunizing first responders and essential workers, like teachers, schools are not entirely without options to pivot themselves. In many districts, this decision by health departments is simply shifting the prioritization scheme for who among school staff will go first.
The emphasis is now to focus first on older employees and those with chronic conditions (personal risk), as well as the aides and staff in high-risk classrooms of children with special needs, for whom an unvaccinated caregiving staff would pose some risk for exposure to the children themselves (occupational risk). Working closely with health departments, there remains ample room to initiate vaccination, assuming counties receive increased inventory in the coming weeks.
Schools are at Various Stages of Reopening Plans, and Testing Programs Can Help
In recognizing the success some schools have had in returning to in-person learning, we also acknowledge that certain districts, particularly those in urban areas, are home to school buildings that are insufficiently equipped to implement all recommended prevention measures. These schools were not able to open for in-person learning during the COVID-19 surges we experienced this fall and winter. However, now as incidence rates continue to decline, we believe these schools can begin to take steps toward reopening for in-person instruction in a graded approach, perhaps starting with students least able to learn effectively through remote technologies.
We are also confident that school-based testing programs can be incorporated into a school’s multilayered plan, providing an additional layer of protection for those individuals coming to school. Through Project: ACE-IT, a collaborative program with local health departments and educational leaders across the five-county southeastern Pennsylvania region, we recently launched an effort with the School District of Philadelphia to provide weekly assurance (or surveillance) testing for teachers, starting with those who work in elementary schools. We will focus on monitoring linked school transmission as a critical metric for school safety, and are excited to implement a program we believe will provide an additional layer of protection in their path to reopening. (The same rapid antigen tests we are using for Project: ACE-IT are becoming increasingly available to the public; we have created an efficient mechanism to provide in-school testing that avoids disruptions to the school day. If that can be helpful to others in establishing similar programs, feel free to use our materials and reach out for guidance.)
We also recognize that some public and independent schools are at a place where they are discussing a move from partial in-person to full in-person instruction. For these schools, incremental expansion of in-person learning seems the best path toward success as it allows for school officials to observe, in a controlled way, how their safety protocols stand up against increasing school populations. Assurance testing programs can also be an important additional tool in these scenarios, as it allows for the identification of asymptomatic COVID-19 infection amongst increasing numbers of students and staff, which can lead to prompt isolation and avoidance of further transmission.
No plan can entirely eliminate the risk of spreading COVID-19 from a school building. However, the knowledge that we have accumulated since the fall supports the success of multilayered approaches to mitigating in-school transmission. Coupling these safety plans with the additional protection of assurance testing programs should provide ample security to school communities, and a sense of optimism that schools can begin their journey back to normal.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia, and is a co-author of PolicyLab’s Policy Review: Evidence and Guidance for In-person Schooling during the COVID-19 Pandemic.
