COVID-19 Outlook: Looking Ahead as a New Administration Takes the Helm

Similar to last week, this week’s update to our COVID-Lab forecasting models reveals much of the country to be in a transition period during a winter surge:
-
Testing positivity rates continue to decline nationally, down from an average of 15.3% last week to 12.7% this week across all of the 819 counties we follow in our model. These declines were evident in nearly all states (48 of 50).
- Testing positivity is falling throughout Arizona, and projections from Southern California to Arizona suggest while high overall case incidence may continue over the next four weeks, these areas might expect declines in overall transmission rates in many counties.
- In the Mountain States, testing positivity rates are stabilizing (Utah and Nevada) or declining (Colorado). A note of caution remains for ski destinations, as some of the region’s highest reproduction numbers (R), a measure of transmission, were detected in Eagle County, Colo. (Vail, median R 1.37), Summit County, Utah (Park City, median R 1.27), and Blaine County, Idaho (Sun Valley, median R 1.68).
- Reproduction numbers are finally beginning to decline around north Texas, as hospitalizations are reaching peak or just beyond. In south Texas, however, we are projecting that reproduction numbers will remain above 1.25 in Abilene, Austin, Brownsville, Houston, Laredo, and San Antonio, causing these areas to lag behind their northern counterparts.
- Despite improvements in many areas over the past week, case incidence remains high in other regions with some counties still not past their winter peaks. Our model projects growth in case numbers for parts of northern California, although at slower rates of growth than in prior weeks, and in the southeastern states of Florida, North Carolina and South Carolina.
- Like the Southeast, the Northeast continues to witness high overall case incidence. Fortunately, our model forecasts that case incidence in upstate New York and many areas of New England will soon move past their peak. We are also encouraged to see slowing case incidence growth rates in some of New York City’s boroughs (Manhattan, the Bronx and Staten Island) with a decline in testing positivity.
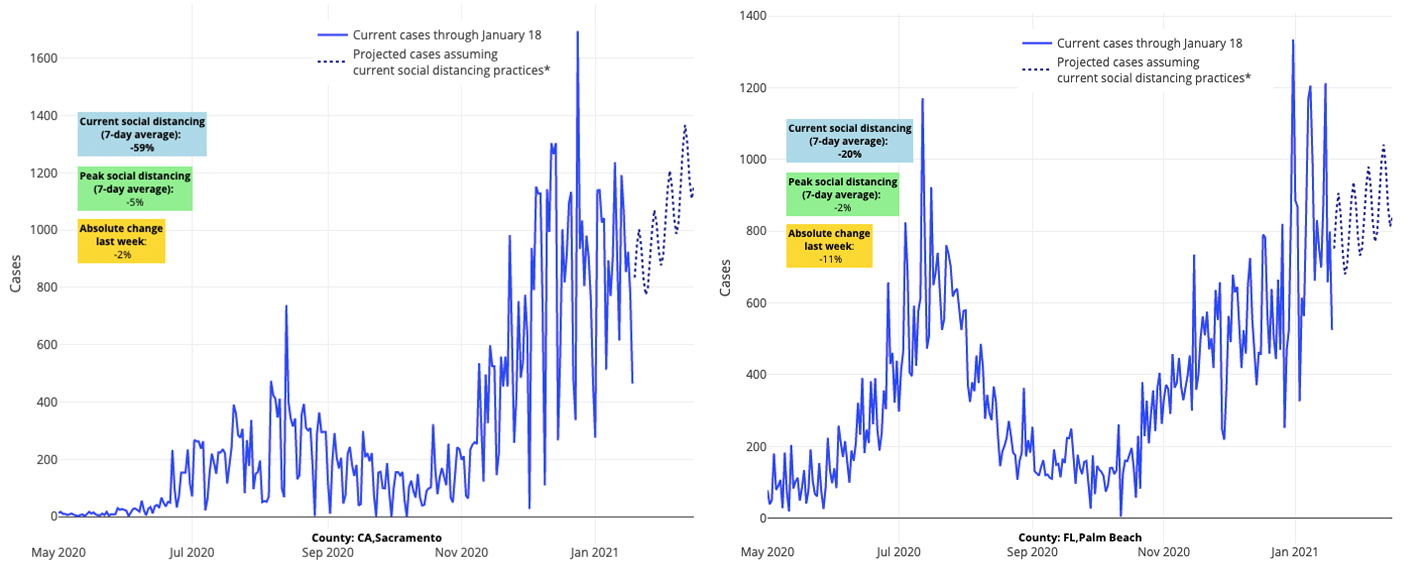
Above are the projections for Sacramento County in California (left) and Palm Beach County in Florida (right).
Cautiously, We Believe the U.S. is Rounding a Corner
A second week of encouraging data trends and projections lends greater confidence that the country may, as a whole, be rounding a corner. Even a review of state death rates suggests we are moving past a national daily peak in mortality in most states.
However, we are cautious not to overstate our optimism. After all, there is evidence for increased transmission in winter vacation destinations, such as Vail, Park City and Sun Valley. We will be observing in the coming weeks whether such time-limited transmission related to winter travel may confer new risk to broader areas, but for now, these projections are outliers within their states.
We are also watching coastal areas of the Southeast, where projections suggest case incidence may continue to worsen well into February. This is potentially related to annual migration of people to these areas, attempting to escape winter weather.
Our optimism is further tempered by continued concerns regarding novel variants and their potential to increase case incidence again. It is not clear that these variants will alter our current transmission rates as there are so many factors at play that dictate transmission beyond the variant itself. For now, we are reassured by these reassuring recent trends and projections, but will keep a close eye on this ever-evolving situation.
What the Next Six Months Could, and Should, Look Like
As the Biden Administration takes the helm this week, we have been considering the most effective strategies a new administration could take to hasten the end of this pandemic. First and foremost, we need to broaden the scope of our thinking. During the next six months, our discussions will need to include developing plans to manage recovery, while at the same time maintaining efforts to control transmission. It would be best if the media and our leaders begin to discard messages that portray the future simply as dire (when it is not), as messages of doom and gloom are likely to lead to more apathy among the public rather than stimulate a mindset that we have the tools and abilities at hand to rapidly reduce case incidence. These efforts include strengthening our resolve for continued mask use and social distancing and ensuring distribution and uptake of vaccines. The warmer months are not too far off, which will bring benefits as well. This combination of factors provides the opportunity to change our fortunes for the rest of this year. However, this optimistic vision will only happen if we learn from the mistakes of the past year, and tackle the challenges of these next few months with bolder plans.
Here are our recommendations of the most effective strategies that the new administration, state leaders and public health departments could adopt over the next six months, as they continue to support/enforce masking:
Vaccinating as Many Americans as Possible
We must admit failure up to this point on vaccine distribution and quickly hit reset. We would applaud a pivot to engaging the National Guard, the invocation of the Defense Production Act, to speed up production and distribution of the vaccine, as well as the new administration’s plans to open mass vaccination centers. However, we must also recognize that many will not be able to visit mass vaccination centers, in particular those individuals living in densely crowded locations that are a harbinger for outbreaks and who have experienced disproportionate impacts from the pandemic. Plans to embed these centers within these communities, allowing for easy access to vaccination, will be vital to halting the transmission of this virus.
Pivoting on Public Messages
We need more clear and consistent public messaging, particularly around continued mask use, social distancing and vaccine acceptance. Messaging aimed at overcoming vaccine hesitancy will need to be customized for specific populations, as the reasons for hesitancy may vary by community. Engaging the help of local news and well-regarded community leaders will be key to this effort. The "Sleeves up, NOLA" campaign in New Orleans is a perfect example of a potentially impactful local effort.
Utilizing Assurance Testing
Even as we rush to get everyone vaccinated, we need to scale up assurance testing, or testing that allows for the identification of COVID-19 in people who do not have symptoms but are still able to spread the virus. Given significant delays in vaccine inventory (which are likely to persist well into the spring), frequent testing can still be a valuable tool in achieving viral reduction in the coming months. In the fall, colleges proved that frequent surveillance testing can control viral transmission and allow for maintenance of in-person learning and other activities without also contributing to spread. Similar approaches can be adapted in other school settings and places of business. We need to deploy more rapid point-of-care tests (antigen and molecular) to these locations as we return to in-person activities.
We might also consider monetary incentives to speed up adoption of assurance testing by schools and businesses. For example, monetary reimbursement could be provided to employers and schools who are doing frequent testing; paid sick leave could be guaranteed for individuals who have been exposed to or infected with COVID-19. Such behavioral economic strategies have been under-utilized thus far.
Defining Clear Strategies for Youth
Throughout the entirety of the pandemic, there have been limited cohesive strategies aimed at returning children and teens to school and extracurricular activities. The approach has relied on local responses with limited central guidance or support. With great urgency, our leaders need to prepare clear strategies for protecting children and teens as the pandemic continues.
As noted above, frequent assurance testing in schools (for staff and high-risk students) can be an important tool. This can serve as a bridge for reducing transmission in schools until vaccination studies are completed in children. But we also shouldn’t wait until the vaccine trials are done to prepare for how we are going to vaccinate youth. We need to begin answering the following questions now: Which youth will be vaccinated first (e.g., older children)? Where will we vaccinate them—can it be done at schools? What are the challenges of distributing the vaccine to different schools (i.e., primary schools vs. high schools vs. colleges)? We can’t wait until the vaccines are approved for children to answer these questions.
Considering How We Will Manage a Return to “Normal”
Looking forward, easing restrictions on businesses is going to be an immediate priority, the timing of which may be best guided by a reduction in hospital strain rather than a reduction in case incidence. A reduction in hospitalizations signals many of the highest risk-individuals (older adults and residents and staff of long-term care facilities) have already sustained infection or been vaccinated. We have seen evidence of this in some parts of the country where transmission rates are rising at a much higher rate than COVID-related hospitalizations, such as the Midwest, the Pacific Northwest, inland areas of the Southeast and a growing number of northeastern cities. We anticipate we will see similar trends in many other areas in the coming weeks. Reducing restrictions on businesses as hospital strain lessens can be a reasonable approach if coupled with continued commitment to assurance testing, vaccination roll-out, and enforcement of masking and social distancing.
While we are hopeful to begin “normal activities” in the near future, we need to consider the non-medical consequences of the pandemic, particularly the aggregating psychological impacts of this past year. Rates of anxiety and depression were high before the pandemic, and the experiences sustained over the past year will only magnify this problem. Further, it is likely that a large segment of the public who previously did not have mental health concerns will emerge from this pandemic with anxiety or other behavioral health conditions. We will need a clear and focused plan for managing these mental health concerns—a plan that assures parity in access to care and insurance coverage across all communities.
Strengthening Our Public Health Infrastructure
Based on those countries that experienced greater success in protecting its public during this pandemic, it is clear that a well-resourced public health infrastructure is vital to the response to a pandemic or other major public health threat. While many of our nation’s public health departments have unbelievably dedicated employees, they do not have the necessary resources. Furthermore, we lack efficient and widespread public health communication, which during this pandemic created an opportunity to amplify non-public voices—resulting in a lack of confidence in data and mixed messages shared with the public. Recognizing and addressing these deficiencies at all levels of the government, and in collaboration across agencies, is imperative to re-envisioning our public health infrastructure for a better response to future health threats.
We got a glimpse of the value of this over the summer when a new national data system, HHS Protect Public Data Hub, emerged and forced the level of collaboration and sophisticated data transparency that can more nimbly manage the next public health crisis. Standing up a new national data system during a pandemic is never ideal, but it was critical, and its flaws can be fixed. A nice review of progress on the national data response was featured this week in The Atlantic.
As a new administration comes to Washington this week, we look forward to the new ideas they will bring to managing our recovery and preparing for the future. In the meantime, we urge patience of the American people. While trends in transmission appear to be improving overall, rates remain high, so we need to stay committed to our efforts to reduce transmission. If we as individuals commit to protecting ourselves and others around us, we will hasten our recovery in the weeks ahead.
