COVID-19 Outlook: Finding Safe Harbor, While Looking Forward

Below are our top-line findings from this week’s update to our COVID-Lab forecasting model:
- Nearly one-third of the 821 counties we follow in our model have averaged an instantaneous reproduction number greater than 1.5 over the last week; Two-thirds of the counties have a test positivity rate over 9%.
- We are projecting North Dakota, Wisconsin, and El Paso, Texas—some of the regions with the highest rates of viral transmission in recent weeks—will move past their peaks over the next four weeks. The timing of this leveling out of case counts suggests it takes 10 weeks to get there, which is a cause for concern for many other areas that are still weeks behind. And the tail may be long.
- Our data shows Michigan, Ohio, Pennsylvania and New Jersey are likely entering their worst stretch of the pandemic; Ohio and Pennsylvania are now among the top five states with the quickest growing test positivity rate, exceeding 15% and 10%, respectively, in the last week, which is an increase of more than 35% from the prior week.
- Many locations in the Mid-Atlantic and Southeast regions are seeing concerning increases in incidence. For example, Nashville is now exceeding 400 weekly cases/100,000 individuals and Charlotte is nearing 200 weekly cases/100,000 individuals.
- This fall surge is also persisting in the Heartland. We forecast that Colorado will still be under significant strain over the next four weeks as testing positivity rates continue to climb in nearly all counties; Denver County exceeded 600 weekly cases/100,000 individuals this week.
- Substantial growth is also projected in areas of California. Los Angeles is near 200 weekly cases/100,000 individuals this week, a number we are projecting could double over the next four weeks.
- Parts of New York and Massachusetts are faring better, but still have evidence of increasing incidence. In Essex County (Boston), despite exceeding 300 weekly cases/100,000 individuals, test positivity rates remain stable at 5% and we forecast that this rate will grow much more slowly than other areas. Similarly, New York County (Manhattan) remains near 2% test positivity (with 125 weekly cases/100,000 residents).
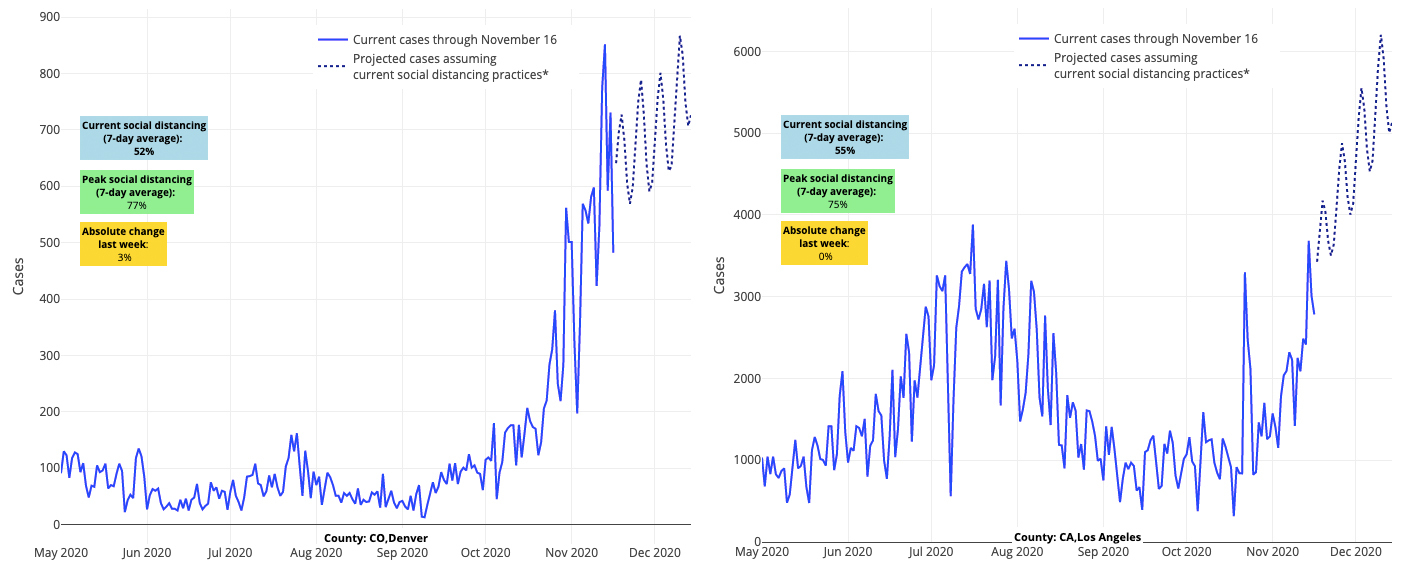
Above are the projections for Denver County in Colorado (left) and Los Angeles County in California (right).
As you can see, the fall surge of COVID-19 continues, and coupled with the holidays that start next week, we believe there will be continued significant rise in incidence across most of the U.S. into mid-December.
Insights Into Our Recommendations
Last week, our weekly blog post included a recommendation that families and communities commit to a collective quarantine before, during, and immediately after the holidays of Thanksgiving, Christmas and New Year’s to try and interrupt transmission during the riskiest season of the pandemic. These recommendations are based on the following facts:
- With areas like Philadelphia now seeing 350 weekly cases per 100,000 individuals, we are witnessing our highest incidence thus far, and it’s occurring just before the holidays.
- Increases in hospitalizations and deaths are following the rise in cases in many states. We are now seeing more than 1,500 deaths per day in the United States with that number expected to rise in the next few weeks, absent significant mitigation efforts.
- Unlike in the spring, children (particularly those ages 11-18) are more involved in this fall wave. At Children’s Hospital of Philadelphia’s testing locations, the testing positivity rate has more than doubled since early October.
- As the case numbers are increasing in our region, schools, as well as congregate care and long-term care facilities, have seen an increase in cases at their locations with reports of transmission within their facilities.
Publicly available data inform these facts and the mitigation strategies we recommend. Community mitigation efforts—principally gathering size limitations, restaurant/bar restrictions and enforcement—should precede any alteration to plans for in-school learning, which should be a last resort.
In the context of accelerating community transmission, remote learning until after the upcoming Thanksgiving holiday provides an opportunity to stop the spread of infection that includes the whole family, given the high positivity rate of children in many areas (particularly those ages 11-18). Yet, since younger children are less susceptible to symptomatic infection, remain in more consistent cohorts, are likely more compliant with in-school safety protocols, and do not have the wider network of social contacts through sports and other activities that older youth do, elementary school and child care could remain in-person. We also continue to advise that students with special education needs might be prioritized for in-school services in small cohorts, given the greater difficulty they may have learning virtually and the services they receive during the school day.
These suggested measures in and around the holidays were, and are still meant to be, time limited. We are hopeful that with a reduction in community incidence, school personnel will be at reduced risk of exposure and can ultimately avoid quarantines so that schools can be fully staffed and stay open. This can help ensure the success of the multi-layered safety plans schools implemented that protect students and staff. And, this is consistent with findings from European studies performed last spring that documented school attendance could be safely achieved despite community transmission.
It is important to note that European studies were performed during a period of significantly lower community incidence than what we are currently experiencing in the United States.
So, Where to From Here?
For COVID-Lab, we are pivoting from a focus on the anticipated winter surge to try and gain a better understanding of when this surge will subside and the recovery can begin. We do this with optimism for a new year, when emerging vaccines, increased access to testing, and the promise of spring should help us quickly gain control of the pandemic, pushing us closer to normal school days.
Up until now, our models have provided four-week forecasts to give communities time to prepare for any predicted increases in case counts. This week, we worked to calibrate our models to better predict when case incidence will begin to trend downwards.
We first assessed the utility of including cumulative prevalence of SARS-CoV-2 test positivity (as a proxy for seroprevalence in a region) in the model. Many will be surprised to learn that inclusion of cumulative test positivity results did not add much information to our predictions. This is likely because variables currently in the model capture the natural case incidence growth of a county and region (for the researchers, our local random effects) that serves as a proxy for seroprevalence. Therefore, we chose not to include a measure of cumulative incidence in our model.
Next, we assessed a “day of week” covariate to account for significant variation in case counts from one day to the next. For example, we usually see increased case counts on Mondays after decreased testing over the weekend. This early week increase can mask other indicators—like improving testing positivity rates and prior-day trends that would suggest areas are moving past their peaks. The addition of this variable is important, as it will allow us to anticipate the downward “turn” more quickly. This addition to the model will result in a more jagged trajectory in our graphs (see example below).
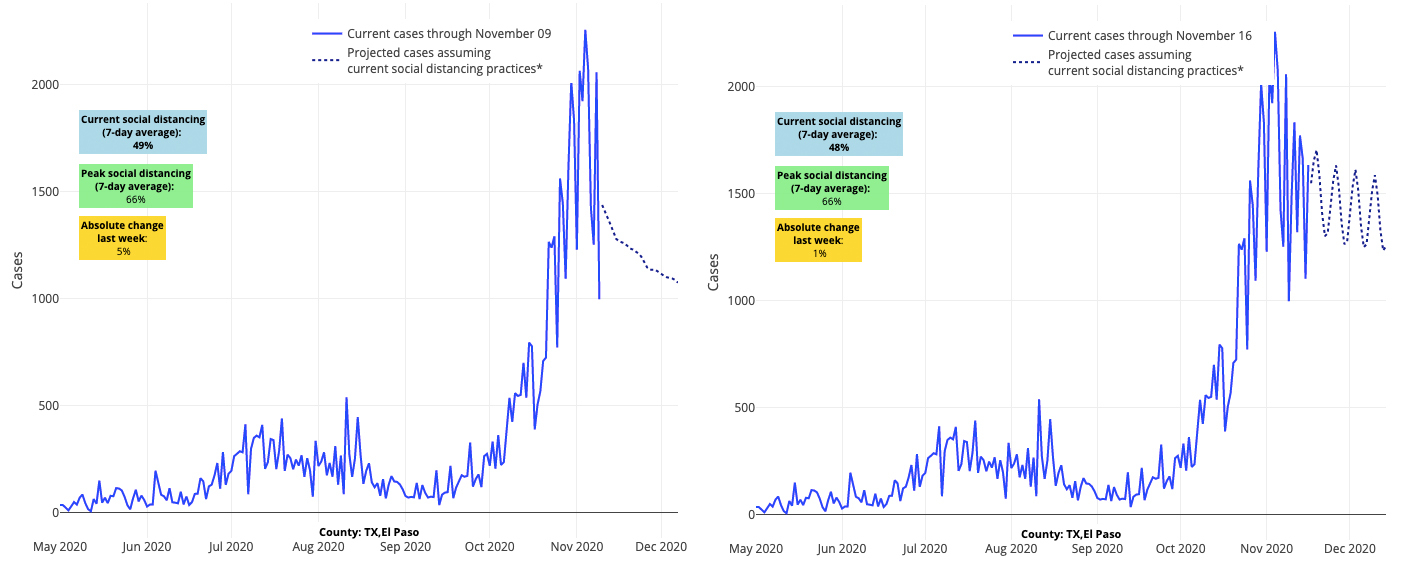
Above are the projections for El Paso County in Texas from the week of Nov. 11 (left) and the week of Nov. 16 (right).
With many states and localities across the country quickly imposing new restrictions to try and manage their highest case counts to date and to limit the burden on their local health care systems, it’s that downward “turn” after the peak that we are all seeking.
As we move through this difficult period and towards a spring of (hopeful) recovery, let’s all keep a sense of optimism that if we remain vigilant in the practices we know can mitigate COVID-19 spread—such as masking, distancing and hygiene—and implement mitigation strategies that work within our communities to suppress the spread, we can protect one another and get through this together. As we begin to buckle down for the holidays, we wish everyone a safe and healthy holiday season. This surge may feel defeating, but we are moving over the top of the mountain, and there will certainly be better days ahead.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia, and is a co-author of PolicyLab’s Policy Review: Evidence and Guidance for In-person Schooling during the COVID-19 Pandemic.
