COVID-19 Outlook: Finding Our Bearings After Labor Day
Just like that, summer has come to an end, and we are bracing for whatever may come next in this pandemic.
This week’s projections show that the Midwest will continue to struggle as we enter fall. Minnesota, Wisconsin, and Illinois, in particular, have captured our attention, not only because they have some of the most concerning case counts in the country, but also because they will soon see colder weather, driving people indoors and potentially introducing a transmission dynamic we have not seen since last winter.
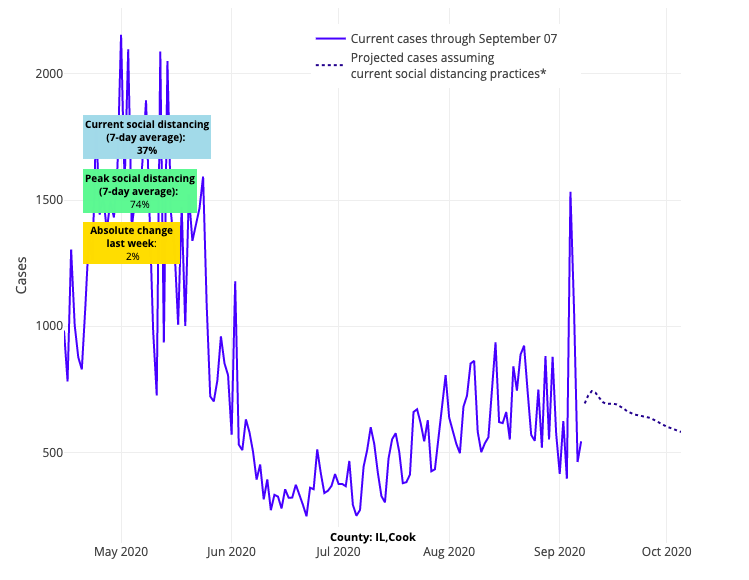
Above are the projections for Cook County in Illinois.
Some of the most impacted regions from summer are showing signs that their resurgence may not be over. For example, Pima, Pinal, and Maricopa Counties in Arizona experienced simultaneous increases in transmission risk for the first time in many weeks, signaling a need to watch reopening strategies, and San Diego, Imperial and Kings Counties in California are also expected to see spikes in case counts over the next four weeks.
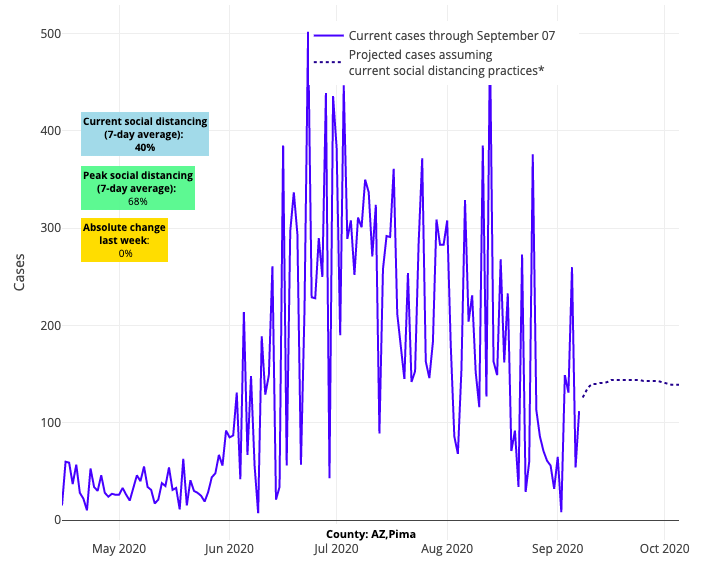
Above are the projections for Pima County in Arizona.
And finally, while counties across New England and New York had improving or stable projections this week, much of the Mid-Atlantic region, from Virginia to southern New Jersey, is seeing increased risk again, including Richmond, Baltimore and Philadelphia. Test positivity is rising widely in the region.
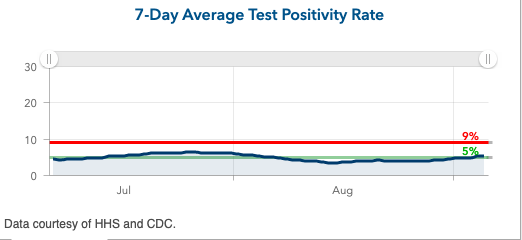
Above is the 7-day average test positivity rate for Baltimore County in Maryland.
We will learn a lot in the next couple of weeks as data emerges after a Labor Day weekend that included lots of travel and gatherings in some areas and from the community impacts of college campus outbreaks. In the coming weeks, an important concern for communities adjacent to college campuses is the potential for a “one-two punch”—experiencing a college-driven outbreak and then being hit by community clusters spurned by Labor Day celebrations. Nevertheless, here are the issues we are considering as we continue to offer projections for the fall:
The Potential Runway for Younger Children to Return to School
We have received a lot of attention on PolicyLab’s updated school reopening guidance that we published in August, which provided both the essentials for strong school safety plans and recommended thresholds of declining case incidence and test positivity to help inform individual school reopening decisions. Many of the comments we received were appreciative of the thoroughness of the guidance, but we also heard frustration that we did not more aggressively lobby for children to return for in-school instruction, irrespective of the case transmission in the community.
As pediatricians and pediatric health experts, we certainly strive for a scenario in which all children are back in school because of the health, social, and economic benefits in-school learning offers to children, families and teachers. However, this needs to be done in a safe manner and under a plan that is endorsed by all involved—parents, teachers, health care workers, public health experts and policymakers. It does not mean transmission risk in a community or school needs to be zero to reopen, but teachers and staff need to feel confident that their fears are being addressed and safety plans can be properly carried out, creating as little additional risk as possible to their health and that of their families. Helping schools feel prepared to reopen requires a focus on how to interpret evidence and feasibly implement infection control practices, as these have been key information gaps for school leaders and staff. We have had constructive partnerships with school districts, teachers and families around how best to safely return children to the classroom.
With this context in mind, we are supportive of plans to return elementary school children and those with special learning needs to the classroom first as the evidence continues to show younger children are less susceptible to severe impacts of COVID-19. This incremental step could build confidence for or identify gaps in school safety plans, allowing older youth with potentially higher transmission risk to return once we learn what is most effective.
Evolving Data on COVID-19 Morbidity in Children
While younger children still appear to be at lower risk for severe disease, it is important to note that our team of pediatricians and infectious disease and public health experts does not feel that we have enough evidence to assume we know how school reopenings will play out in terms of COVID-19 transmission risk and child morbidity. Most evidence on COVID-19 and children that has accumulated to date has occurred in the context of children being sheltered from much of their normal interactions within society.
With the coming winter and potentially associated risk for other viral infections like influenza, it would be premature to make comparisons of risk. Already, Florida is reporting infections among school-aged children have increased by 34% since schools opened last month. Closely monitoring the morbidity of these infections and determining whether we are seeing different transmission dynamics in school settings will be important. So, too, will be a similar analysis of how the spread of the virus changes as the weather turns colder. At the same time, we are continuing to learn about rare, but important complications in young athletes, such as myocardial inflammation, which requires further study.
The bottom line: our understanding of COVID-19 and children is still evolving. Therefore, any and all plans to move forward with in-person school and return to athletics need to be done in a measured way with a close eye on the evidence.
How Well Colleges Can Contain Outbreaks
Very few, if any, colleges across the country did not see a COVID-19 outbreak upon move-in for the new semester. While these early outbreaks were not surprising, the resulting severity of the outbreaks among students and transmission risk to the surrounding community has been mixed. Even as we see in our projections the risk of community spread to neighboring counties for some college towns, like State College, Pa., Fayetteville, Ark., and Tallahassee, Fla., we also see universities that are gaining control of their outbreaks. This includes relative stabilization in South Bend, Ind. (University of Notre Dame), improved projections in North Carolina’s Research Triangle, which saw significant outbreaks at the University of North Carolina and North Carolina State University, and relatively little concern for continued transmission risk from Purdue University, the University of Michigan and Duke University.
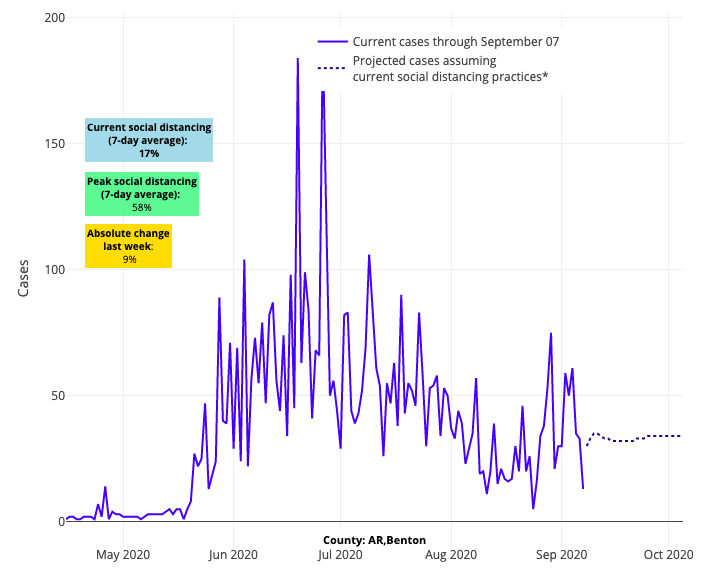
Above are the projections for Benton County in Arkansas, which is a neighboring county of Fayetteville.
Finally, colleges in Vermont have largely opened without problems, confirming that low community case incidence is the best antidote to safely reopening.
Now comes the true test of universities’ mitigation plans that they worked so hard on this summer and continue to adapt. Challenging even the best mitigation strategies will be factors such as the amount of disease already existing within these towns and the extent to which the institutions are cloistered vs. integrated into the larger community. Despite these challenges, a number of colleges have succeeded thus far with their return to school and so it is clear that an extended outbreak on campus is not a predetermined event.
If our colleges can succeed with protecting perhaps the highest-risk individuals in their community (or if those individuals can safely protect themselves while able to continue their own pursuits), then surely many of our high schools might succeed as well. The upshot is that if colleges can be successful this fall, we should be bullish on safety plans for not simply our younger children, but for our high schoolers as well.
What’s Going on With Hospitalizations?
We have been encouraged to see hospitalization rates stabilize even as cases have risen among younger people in many locations. We see this in Minnesota and Illinois, even as their cases have continued, and are projected to continue, rising in recent weeks. We suspect that that mismatch of hospitalizations to case incidence confirms that most infections—milder in nature—are now occurring in younger, healthier individuals. It raises the potential that communities and individuals themselves have been able to isolate the highest-risk individuals among us as we return our children to schools and other sectors of the economy continue to reopen.
It remains conceivable that if people commit to practicing the fundamental safety precautions of masking in public locations and limiting the size of gatherings, we can find our way through this crisis with schools open, and many areas of our economy returning safely. However, the big unknown here is the contribution of colder weather to this assessment. The findings in our July JAMA Network Open study revealed the efficiency of this virus to spread—and with potentially higher virulence—during colder weather months. That’s why as we try to accommodate to our new normal, we must not let our guard down with regards to masking, hygiene and distancing. The big test is still coming.
So, we leave you this week hopefully with a sense of cautious optimism. That even as we may see continued transmission past Labor Day, we should also not discount the unexpected improvements in some college towns, the stabilization of hospitalizations in many areas and some improving consensus around safety plans in schools.
These are our new bearings after the holiday weekend, even as we await the uncertainty of the winter ahead.
Gregory Tasian, MD, MSc, MSCE, is an associate professor of urology and epidemiology and a senior scholar in the Center for Clinical Epidemiology and Biostatistics at the University of Pennsylvania Perelman School of Medicine. He is also an attending pediatric urologist in the Division of Urology at Children's Hospital of Philadelphia.
