COVID-19 Outlook: Planning for Summer as Case Incidence Continues to Decline in the U.S.

In this final week of our weekly COVID-Lab modeling forecasts, here are the latest national data:
- Nationally, the average PCR testing positivity rate declined to 4.2% over the past week (down from 4.9% last week). Seventy percent of the 821 counties included in our model have a testing positivity rate below 5%; those above 5% are concentrated in the Midwest, South and Mountain States.
- The average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) remains below 1 (0.96 this past week); only 21% of the counties we follow had reproduction numbers above 1, which indicates increases in case incidence.
- Average weekly case incidence across the country declined to 73 cases per 100,000 individuals, with only one-quarter of all counties seeing more than 100 weekly cases per 100,000 individuals. Locations continuing to see higher case incidence (200+ weekly cases per 100,000 individuals) include Tacoma, Wash., Birmingham, Ala., Greensboro, N.C., the Denver metropolitan area, South Bend, Ind., and Shreveport, La.
This week’s regional updates:
- Steep declines in case incidence and hospitalizations continue throughout the Northeast and Mid-Atlantic, and our forecasts show continued declines in cases over the next four weeks.
- Even as our models predict case incidence will continue to decline in Denver County, improvements in the collar counties and Colorado Springs are moving more slowly. Furthermore, COVID-19-related emergency department visits have not yet declined across the entirety of Colorado.
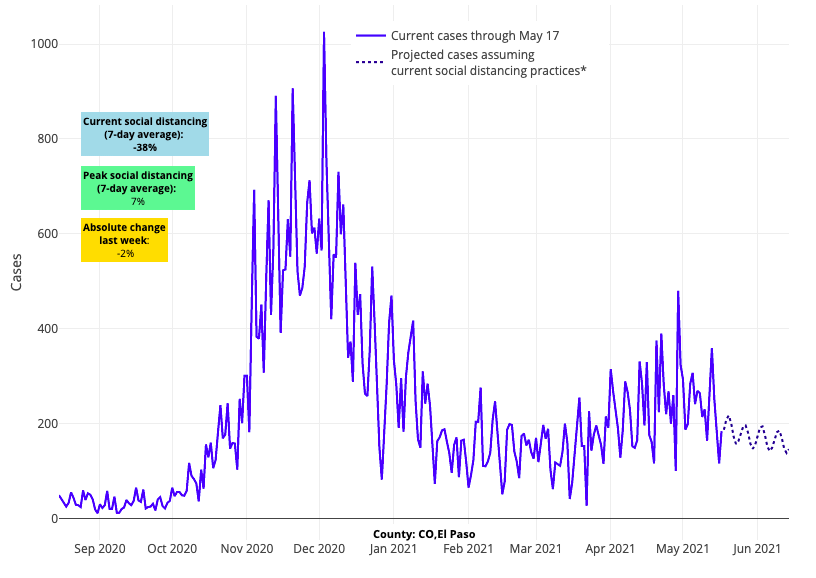
Above are the projections for El Paso County (Colorado Springs) in Colorado.
- Hospitalizations remain stalled at seasonal peaks throughout Northwest metropolitan areas of Oregon and Washington. Forecasts are more favorable for Portland than for Tacoma, where test positivity continued to rise this week. Washington is one of the few states with growing a test positivity rate.
- With low vaccination rates overall, the major cities in Louisiana bear watching—testing positivity is more uniformly rising in these locations and our projections forecast sustained higher case numbers in advance of Memorial Day weekend.
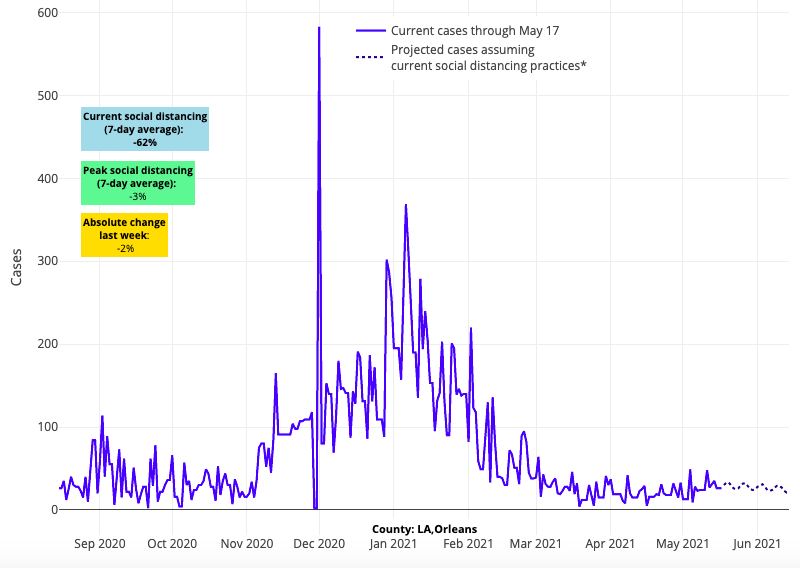
Above are the projections for Orleans County in Louisiana.
- Alabama is seeing the highest reproduction numbers in the country, as community transmission increases and hospitalization rates remain flat or slightly elevated.
As we head toward Memorial Day weekend, we are in a very different place than we were a year ago. Our models show that transmission will continue to decline around the country, led by regions that have achieved high vaccination rates.
However, even as case incidence more quickly improves in regions with high vaccine uptake, the national decline in case incidence is likely to be slow with a long tail attributed to smoldering transmission—most likely from decreased mask use in areas with poor vaccine uptake. Regions of concern remain throughout the Midwest, Southeast, and parts of the Southwest, where vaccination rates have not kept up with the pace of communities reopening. We are also seeing new evidence that the sustained transmission Colorado has experienced is spreading to Wyoming, Montana, and New Mexico, where our models now project sustained case incidence over the next four weeks.
Hopefully, the recent Centers for Disease Control and Prevention (CDC) decision to lift masking recommendations for the vaccinated will lead to improved vaccination rates in these more vulnerable areas. But all told, as numbers continue to decline, the risk for families is far less than it was a year ago, and we would suspect that while we might see some increasing transmission after the holiday weekend, it will be far less than what we witnessed last year.
What’s next for K-12 schools?
This past week’s CDC announcement that fully vaccinated people can resume activities without wearing a mask or physical distancing is a welcome message for many. However, it left some school leaders scrambling to update their plans for the remainder of the school year. This is especially true for graduation ceremonies, as many schools had planned to limit attendance to only a few family members, while also requiring attendees and students to wear masks.
It would not be surprising to see many schools adhere to their plans and finish the school year without changing school safety protocols or event plans. Still, some may see an opportunity to begin allowing vaccinated youth and teachers to attend school without masks, assuming their nurses are made aware of who is vaccinated (as they would be for other vaccine preventable illnesses in a normal school year). Others may see an opportunity to leverage COVID-19 assurance testing as an added layer of protection for late spring events, such as prom and graduation, particularly among those who are unvaccinated.
There is no one-size-fits-all approach for safety protocols as the school year ends; as has been the case throughout the pandemic, it all depends on the individual school, the risk tolerance of their school community and their experience since fall.
Preparing for summer camp
Many summer camps that weren’t open last year are reopening this season. With that in mind, the CDC released guidance in April recommending masking and physical distancing as mainstays for all individuals (staff and attendees) at this year’s summer camps. However, these camp-specific guidelines are at odds with the more recent recommendation to lift mask and social distancing requirements for vaccinated individuals. Furthermore, a blanket approach to mitigation guidance ignores the uniqueness of each camp.
In reality, camp leaders will need to consider several factors in developing a mitigation strategy that is ideal for their setting and participants. They will also need to remain flexible as case incidence continues to change throughout the summer. Here we offer a number of questions that camp leaders might consider as they develop their strategy:
1) What are the community test positivity and incidence rates in our area, and is transmission projected to increase or decrease in the coming weeks? Unfortunately, there are no evidence-based thresholds for test positivity or weekly case incidence below which it is deemed completely safe to abandon mask use. In some ways the risk will never be zero. However, if test positivity and community transmission rates in your area are very low and declining the likelihood that any one individual (vaccinated or unvaccinated) will get exposed to SARS-CoV-2 will be low. Knowing your local rates can help inform initial plans and adjustments along the way.
2) Are a significant proportion of participants and staff vaccinated? All children, ages 12 and above, and all counselors will have had the opportunity to be vaccinated before summer. As camps hire over the next month, some may choose to prioritize counselors who have been vaccinated. Particularly for sleepaway camps, a fully vaccinated staff can permit greater flexibility for counselors to spend time away from camp on days off and can greatly reduce the likelihood of outbreaks upon their return. If the camp is for older children and the vaccination rates are high among staff and participants, then it would be very reasonable to eliminate mask requirements.
3) What if the majority of children attending the camp are under 12 years of age? Because vaccines have not been approved for use in children under 12, any camp servicing this age group will have an unvaccinated participant population. In this circumstance it is likely, and very reasonable, that camp leaders will require masks for these younger campers. However, mask requirement for these children should be revisited throughout the summer. If case incidence drops to very low levels in the community and the staff vaccination rate is high, then it would be very reasonable to consider relinquishing mask requirements. It is also important to consider the location of activities at the camp (see #5 below).
4) What if my camp has children with underlying health issues? There are many camps that offer experiences for children with medical conditions that may impact their risk for severe infection from COVID-19. In these circumstances, camp leadership should engage with medical personnel when developing their safety protocols. Depending the on specific population of children, protocols might include mask use and/or testing, especially if community transmission rates remain elevated.
5) Are the camp activities predominantly indoors or outdoors? Until community transmission rates are very low, mask use is likely to continue being recommended for indoor activities, especially if the majority of children in attendance are under the age of 12. However, transmission outdoors is far less likely than indoors. While the CDC guidance for summer camps is that children should wear masks while playing or congregating outdoors, we are not convinced that this is necessary even for younger unvaccinated children, especially if adult staff are vaccinated. It is likely that CDC guidance on this topic will be updated this summer.
6) Can testing be used as an adjunctive tool to open camps? Testing is now widely available and relatively time and cost efficient. Therefore, some camps, especially overnight camps, may opt to screen campers when they arrive as a way to prevent outbreaks. Boarding schools and college campuses showed us over the past year how effective this type of testing can be. The value of testing will be greater for communities in which transmission has not yet abated. Should community transmission continue declining rapidly, assurance testing may not prove necessary.
7) What is the risk of bringing together unvaccinated children at camp? The risk of infection will persist for unvaccinated individuals and certainly may increase for unvaccinated children attending camp with other unvaccinated children. However, such infections are often not severe and, thus, parents may reasonably conclude the benefits from attending camp are greater than the risks. Importantly, throughout this past year, strict safety protocols for children congregating in places like schools were necessary given the risk that they could spread SARS-CoV-2 to unvaccinated school staff and family members. Now that staff and caregivers of schools and camps have received or at least been offered vaccination, the need to strictly enforce safety protocols among children has changed. Camp leaders and parents of attendees will have to consider this new risk-benefit equation when considering mask requirements for their children.
We suspect that many camps will look fairly normal this summer, even if many children remain unimmunized before fall. This is the reward for a pandemic that is finally abating. And it is an important moment in a journey back to normal that accepts we are accommodating to a virus that we will learn to live with as it becomes less omni-present, particularly for those who have been vaccinated.
Acknowledging the team behind COVID-Lab
As our weekly forecasts sunset this week and our team transitions to periodic updates, we would be remiss if we did not note the tremendous interdisciplinary effort that was behind the projections, data analysis and guidance we published each week. Thank you to those involved in PolicyLab’s direct COVID-19 response work, including Lindsay Capozzi, Laura Cavello, Susan Coffin, Sophia Collins, Koby Crammer, Tyler DeRubio, Maggie Eisen, Jeffrey Gerber, Jing Huang, Caroline La Rochelle, Deanna Marshall, Meredith Matone, Jeffrey Morris, Jeffrey Pennington, Radhika Purandare, Rebecka Rosenquist, Kathryn Saulinas, Lihai Song, Vicky Tam, Gregory Tasian, Lauren Walens, Xi Wang and Zi Wang. We’re also grateful for the contributions of our many colleagues across PolicyLab who have been monitoring the indirect impacts of COVID-19 and child and family well-being; you can view their important work on our COVID-19 resource hub.
We hope that our analysis and interpretation was helpful in responding to the uncertainties of the COVID-19 crisis. We are thankful for all the policymakers, public health leaders, school leaders, school communities, and families who have allowed us to help navigate this journey with you, and we wish you all brighter days ahead.
