COVID-19 Outlook: A Nation Improves, But Challenges Re-emerge in Some Regions

With the news this week that vaccinations for school-age children are likely to arrive this fall, our COVID-Lab modeling team reviews the current landscape across the 821 counties we monitor, along with how this new development could impact transmission around the holidays, starting with Halloween.
Here are this week’s national updates:
- Nationwide, average PCR test positivity is 11.2%, down from 12.5% last week. Despite the overall decline, one-quarter of the 821 counties we monitor had higher test positivity than the week prior.
- The nation’s average reproduction number (a measure of transmission that estimates how many additional individuals, on average, will be infected by every positive case) is hovering just above 1. This is resulting in a relatively stable average weekly case incidence of 367 cases per 100,000 residents.
Here is this week’s regional and county-level assessment:
- More than one-third of all counties in our model have case counts over 400 cases per 100,000 residents. Counties with the largest increases in weekly case incidence are concentrated in the northern regions of the country, including Alaska, Montana, Minnesota, Wisconsin, Iowa and Michigan. Adult and pediatric hospitalizations are also increasing in these locations.
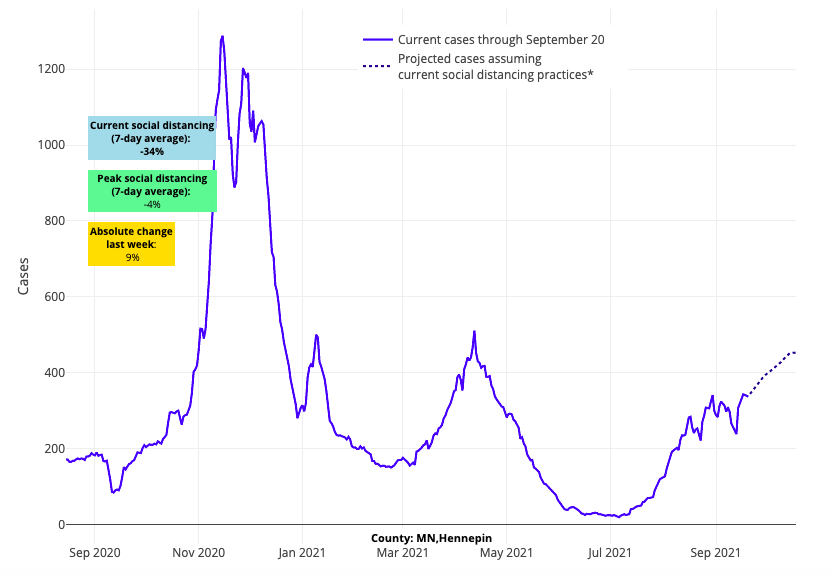
Above are the projections for Hennepin County in Minnesota.
- In Massachusetts, our models forecast growth in case incidence for major metropolitan areas in the coming weeks, though notably, this projected increase is not as brisk as the trends seen last year. Adult hospital census in this region is increasing slowly, while state pediatric hospital census remains at only 10 children (up from 5 children in the last few weeks).
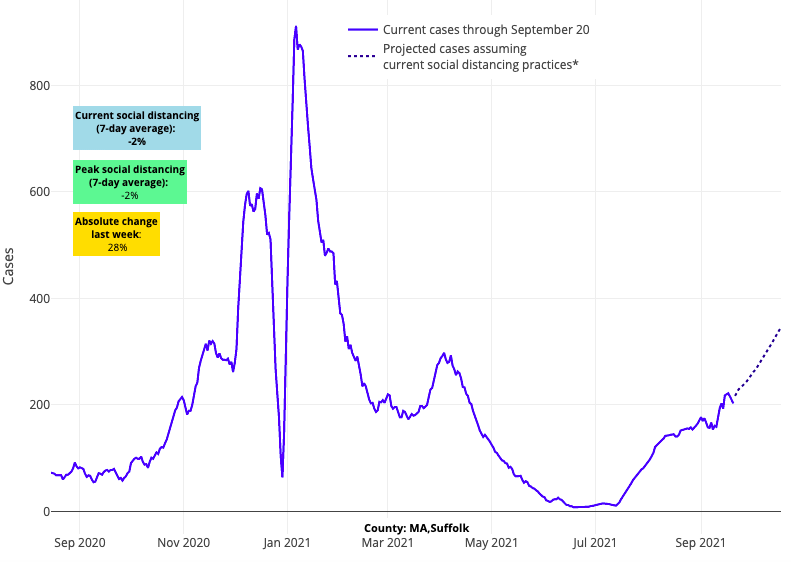
Above are the projections for Suffolk County (Boston) in Massachusetts.
- Case incidence is increasing rapidly in Maine, and hospitalizations have surged to levels reminiscent of last winter’s peak. Similarly, Vermont is demonstrating increased transmission and hospitalizations, but thus far adult hospital census remains under 50 individuals in the state and is below last winter’s levels.
- In the Mid-Atlantic region, reproduction numbers hover around 1 along the I-95 corridor from Baltimore to New York City. Just to the west, however, increasing case incidence and reproduction numbers in the rural areas of Pennsylvania and Maryland bear watching in the coming weeks.
- Washington, D.C. stands apart from other cities in the Northeast for rising transmission alongside rising adult and pediatric hospitalizations. It is unclear how long this risk will continue, given that the collar counties in Virginia and Maryland show evidence of stabilization this week with flat, but high, case incidence forecasted in the coming weeks.
- Texas is a tale of two regions. As the southern metropolitan areas improve, northern Texas (led by the Dallas area) is again struggling with increasing case incidence, and our models project this trend will continue in the coming weeks.
- The greater Southwest continues to show signs of stabilization, alongside declining PCR test positivity, reproduction numbers, case incidence and hospitalizations. This includes a large geographic area stretching from Arizona to California to Nevada.
- Reproduction numbers and case incidence are declining throughout the Pacific Northwest between Portland and Seattle. Declining adult and pediatric hospitalizations are following quickly behind.
- Declining transmission in the Southeast continues unabated this week and is extending northward into the upper South, particularly in communities across Georgia and Tennessee.
Declining transmission evident throughout the Southeast, Southwest, Mid-Atlantic and Pacific Northwest
Local case incidence metrics this week substantiate our model’s previous projections predicting a decline in case incidence across the South and up into the Mid-Atlantic. Not only are areas throughout Florida, Louisiana, Mississippi, Alabama and southern Texas improving, but this trend extends further north to include Georgia, the Carolinas, Tennessee and Kentucky. This improvement across a vast geographic area is bringing a summer resurgence—that resulted in more daily deaths for the South than were observed in winter of 2020—to a conclusion. In the West, continued improvements are being seen in California, Arizona, Washington and Oregon as they move beyond their summer peaks. As these changes take hold, child hospitalizations have also started to decline throughout these regions, and adult hospitalizations are moving past peak as well.
Emerging concerns on the horizon
While we’re seeing positive developments in several parts of the county, areas of concern remain, and are concentrated in the North. Increased transmission continues in the Mountain West, and our model projects continued growth in the coming weeks. Idaho, in particular, has experienced continued significant increases in case incidence, though our models do suggest the state may be nearing peak transmission in the coming weeks.
Counties throughout Utah, Montana, Wyoming and further south in Colorado have also sustained growth in case incidence in recent weeks. Colorado’s high vaccination coverage (70% of adults fully vaccinated) has likely helped to slow the growth in case incidence and hospitalizations in the Denver area thus far. Denver’s resistance against substantial growth in case incidence stands out for the entire region.
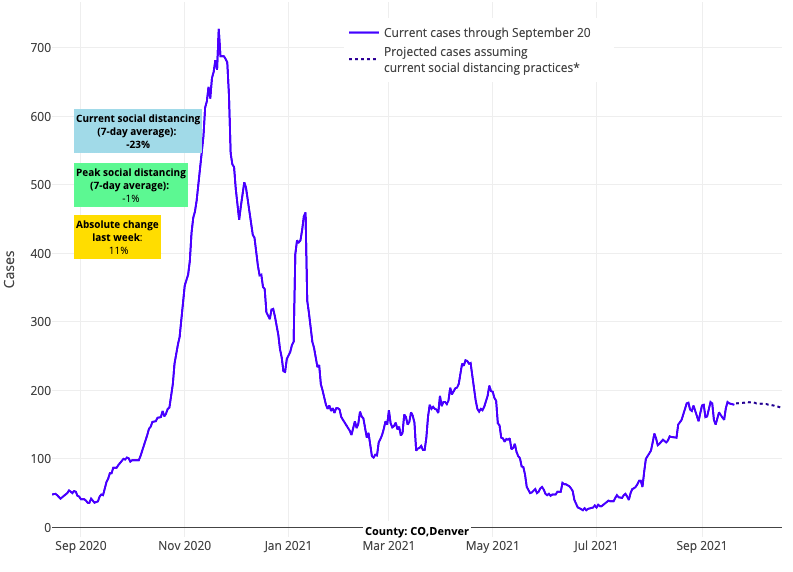
Above are the projections for Denver County in Colorado.
Increasing case incidence is also apparent in the Upper-Midwest including Minnesota, Wisconsin and Michigan. This pattern of growth is similar to what we saw last year for these areas. It will be important to monitor transmission dynamics for areas of Minnesota and Wisconsin relative to other states in the region in the coming weeks. Vaccination rates for both states are in the top half of the country, with nearly 70% of adults over 18 years of age now fully vaccinated. We will be watching their forecasts and hospitalization data (both pediatric and adult) closely, as it is possible that these vaccination rates will blunt their fall/winter surge. We will also be looking at the Northeast, as forecasts for northern New England are consistent with some of these locations in the Upper Midwest.
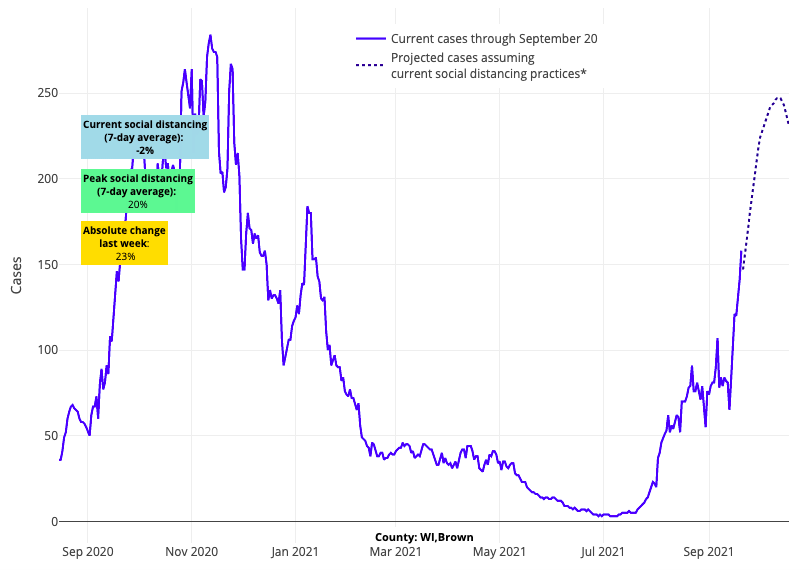
Above are the projections for Brown County in Wisconsin.
Vaccinations for elementary age students likely to arrive in October
While the fall and winter patterns of transmission we are observing may be concerning, rising vaccination coverage can instill optimism that many areas might avert the negative consequences of COVID-19 that some states experienced over the last few weeks. Such optimism received a boost this week when Pfizer submitted data to the U.S. Food and Drug Administration (FDA) to request an emergency use authorization (EUA) of their mRNA vaccine for children between age 5 and 11. The FDA has responded to previous requests for an EUA in a matter of weeks, meaning children in this younger school-age group may be eligible for vaccination as early as mid-October.
The arrival of vaccines for younger children could not come at a better time. Throughout the pandemic, holiday gatherings have consistently precipitated accelerated COVID-19 activity in many communities. While much of the focus in 2020 was on Thanksgiving and Christmas gatherings, we cannot forget the contribution that Halloween gatherings had on COVID-19 transmission last year. In our own region, the largest increases in pediatric transmission occurred a week after Halloween, and the potential for Halloween gatherings to accelerate COVID-19 infections among youth this year remains. With that in mind, a mid-October arrival of vaccinations for younger children is particularly welcome, offering an opportunity to blunt the impacts of the coming holidays, starting with Halloween.
The availability of vaccinations for more children this fall may prove to be a critical turning point in the pandemic for families—but there is much work to be done. We have already seen underwhelming vaccine uptake among children 12 and older in many communities, and poor vaccination coverage has contributed to the large increases in COVID-19 infection among children and adolescents this summer. Currently, fewer than 50% of adolescents have been fully vaccinated.
These numbers serve as a reminder that availability of vaccine alone will be insufficient without attention to educating families about the value of vaccinating children, as well as facilitating easy and prompt access for families to obtain vaccines for their children. Pediatric and family medicine offices will be critical in this endeavor, but we will again need partnerships with our health departments, schools and community pharmacies to enable prompt access needed to maximize child vaccination rates before the upcoming winter holidays.
Many of the unsung heroes of this pandemic are the individuals across all these sectors working tirelessly to provide families and children with access to timely vaccinations, and before that, to needed diagnostic care. This week, we celebrate all these heroes, and send a special shout-out to two of our own: Sophia Collins and Sage Myers. Sophia and Sage were recently recognized by the Philadelphia Business Journal for the incredible dedication they have shown throughout the pandemic to facilitate access to vaccinations for families throughout the Philadelphia region. Alongside them is an even larger group of volunteers who have contributed time and again over the course of the pandemic. We are comforted by the knowledge that they are already planning for the next leg of this journey, as we prepare to offer vaccine access to families with young children who have been waiting patiently for 18 months for their turn in line.
Jeffrey Gerber, MD, PhD, MSCE, is the associate director for inpatient research activities for Clinical Futures at Children’s Hospital of Philadelphia and co-author of PolicyLab's Guidance for In-person Education in K-12 Educational Settings.
