Naloxone is Going “Over the Counter:” Will it Reach Our Kids?
Editor’s Note: This post is part of a series taking a family lens to substance use and substance use disorder through solutions that can support children, teens and caregivers. Through harm reduction measures, public policies, and connections between health care systems and community-based services, the authors offer tangible opportunities to address the substance use crisis impacting families in our community and across the country. PolicyLab developed the series in partnership with Children’s Hospital of Philadelphia’s Comprehensive Opioid Response and Education (CORE) Program. Read “Preventing Pediatric Injury from Medical Opioids.”
There is no doubt that naloxone—a medication that can help reverse an opioid overdose—saves lives. In responding to the opioid crisis, federal, state, and local health authorities have worked tirelessly in recent years to ensure that millions of doses of naloxone have been made available to the public, using creative strategies to remove the standard barriers that interfere with accessibility of prescription medications. For example, all 50 U.S. states have made naloxone available without an individual prescription, usually through state standing orders. Public health and harm reduction programs have used community dispensing models, where naloxone doses are provided free of charge along with overdose reversal education for laypeople.
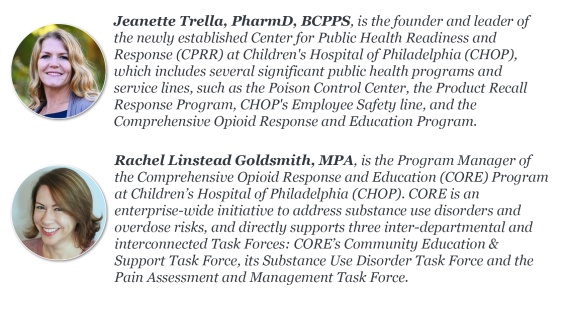
When Children’s Hospital of Philadelphia (CHOP) asked its Poison Control Center leadership to develop a response to increasing opioid overdose deaths in the Philadelphia region in 2019, expanding distribution of naloxone was one of the top solutions set forth in our Community Health Needs Assessment. We have worked closely with Pennsylvania’s Naloxone for First Responders Program (NFRP) while establishing our Comprehensive Opioid Response and Education (CORE) Program here at CHOP, and made naloxone available to families via CHOP’s Emergency Department and at CHOP community events, among other efforts.
We believe that every population in Philadelphia needs more access to opioid overdose reversal medication—including families with children. Poison control centers see the harm presented by children’s exploratory ingestion of a variety of products every day, but a CHOP team recently found that from 2005 to 2018, opioids were the most common substance contributing to child death by poisoning. At a national level, opioids increased from 24% of the substances contributing to child deaths in 2005 to 52% in 2018.
Unfortunately, in the shadow of the COVID-19 pandemic, overdose deaths have continued to rise across all populations. In 2021, the Centers for Disease Control and Prevention (CDC) reported that overdose deaths in the U.S. topped 100,000 annually for the first time. For the same year, Philadelphia reported the highest number of unintentional overdose deaths on record, with 1,276 fatalities; 82% of these deaths involved opioids. In an effort to make naloxone even more available, the Food and Drug Administration approved Narcan® as an over-the-counter (OTC) product in March. Narcan® nasal spray is expected to debut in retail locations this summer.
While this level of approval helps to communicate the safety of this medication and may make it more physically convenient to access, it may also negatively impact the effectiveness of standing order and community distribution models aimed to reduce cost and education barriers. The drugmaker has stated it will aim to price OTC Narcan® at $50 a carton, but for many families, this will still be cost prohibitive. While $50 is less than the full cost of naloxone currently (approximately $125 per carton), without processing it as a prescription, Medicaid and private insurance companies will not be able to be charged to reduce the financial burden on the family.
We encourage our government partners at all levels to ensure the OTC status of naloxone won’t detract from the existing public health infrastructure. We urge them to continue to strengthen naloxone access through the following:
- Educate both health care professionals and the public that naloxone is safe to use in children and should be readily available in households, especially if substance use disorder is impacting the household
- Continue and grow the first responder model for delivering naloxone to those in need. Partner with pediatric health care providers like Pennsylvania’s NFRP has with CHOP, to assure families can receive free naloxone
- Through regulatory provisions, allow for pharmacies to process and charge Medicaid and other insurance plans for a $0 dollar copay for consumers purchasing OTC naloxone
- Consider requiring an add-on naloxone storage system for existing defibrillators and corresponding marketing to educate the public about this availability
- Develop a model to capture data on the methods of naloxone dispensing to help inform future decision-making on the most effective type of access. Leverage America’s Poison Centers to support this data capture
Like a jolt from a defibrillator, every person in need of naloxone should be able to receive it free of charge—including our kids. Additional policy solutions that improve access to this lifesaving treatment even more could help reduce accidental poisonings among children and the burden overdoes are having on our community.