The Role of Health Technology and Incentives in Improving Asthma Care for High-risk Children
Michelle* has severe asthma with frequent flare-ups. She has many environmental triggers—such as weather changes, colds and secondhand smoke exposure—and has difficulty taking her daily controller medication consistently. Her grandmother smokes, though she is trying to quit, and Michelle spends time after school at her house. Michelle’s parents worry that pests and mildew in their house are also contributing, but their landlord is strict about making significant home repairs. They are also worried that Michelle’s school plays a role, as the building is old and hasn’t had proper repairs in several years due to funding shortages.
At Children’s Hospital of Philadelphia (CHOP), we care for many children like Michelle with uncontrolled asthma. Asthma is a leading cause of childhood illness, and it is also a condition characterized by pervasive and persistent racial and socioeconomic disparities in both incidence and severity. In particular, compared with their peers, low-income, non-Hispanic black children have higher rates of asthma, asthma-related emergency department (ED) use and hospitalization and death from asthma.
Many factors such as environmental allergens, secondhand smoke and lower health literacy can impact differences in asthma outcomes. But perhaps one of the most well-documented factors is non-adherence to asthma medication. As health care researchers, we see this as an opportunity for improvement and as one potential way to help close the gap in asthma disparities. How can we help families whose children are exposed to environmental triggers at every turn achieve better asthma control?
Opportunities for Asthma Care Innovation
As we work on approaches to address the social determinants mentioned above and in past blog posts, our team is investigating how technology can play a role in developing better solutions for patients. For those living with asthma, there are several innovative areas that could be particularly helpful including using merged data sources to explore causes of asthma and interactive or “connected” technologies that could assist families with asthma self-management and care.
Initial data for remote monitoring technologies to help manage asthma symptoms is encouraging and has led to a surge of commercial investment in respiratory device monitoring systems (e.g., Propeller Health, Cohero Health, Adherium). These approaches are attractive because they have the potential to help explain and reduce differences in asthma outcomes.
Additionally, prior research has shown that the use of certain behavioral incentive strategies can complement monitoring technology and is an effective way to modify health behaviors in adults. But the question remains, can we apply these concepts to meet the unique health care needs of high-risk children and their families? Examining these opportunities through a health equity lens is critical—otherwise a lack of research and adoption in the populations most affected by asthma threaten to worsen existing asthma-related disparities.
Finding Solutions that Work for Children with High-risk Asthma
We know that racial/ethnic minority and low-income individuals in the U.S. tend to depend more heavily on smartphones to access the internet than other demographic groups. In Philadelphia, where access to broadband internet is severely limited in some neighborhoods, smartphones are often the only way some families can access the internet. Therefore, mobile technology may be an effective way to facilitate health behavior change among underserved populations by engaging with them through apps and text messages.
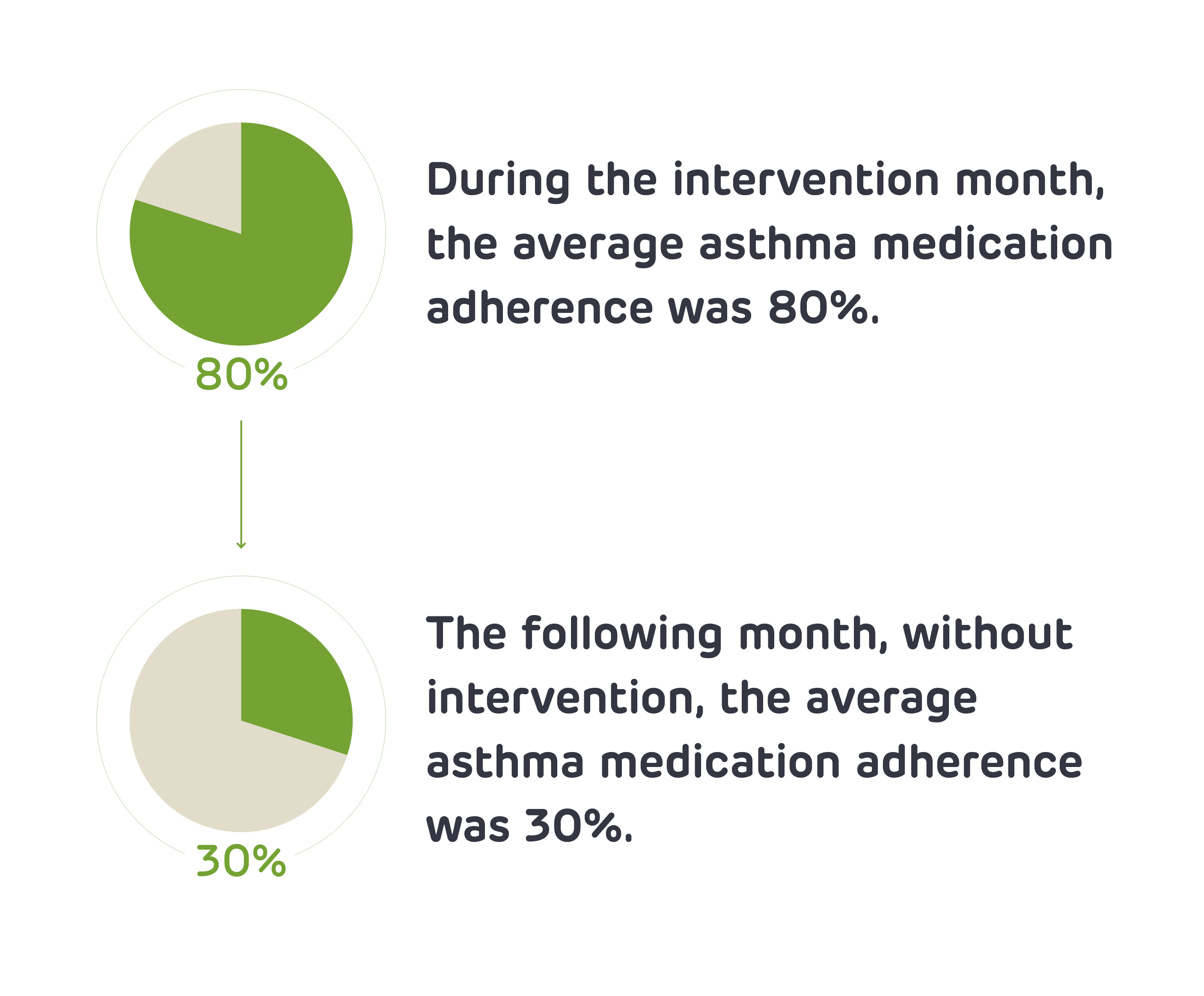
In a recent PolicyLab pilot study, we looked at whether a combination of mobile technology and small financial incentives would be acceptable and useful in improving medication adherence in families of young children with multiple asthma hospitalizations. Children ages 5 to 12 could earn up to $1 per day for perfect adherence and parents received daily medication reminders through an app that was linked to their child’s inhaler. Results showed that almost all of the caregivers surveyed liked the idea of their child receiving adherence incentives and the caregivers felt incentives motivated children to take their daily medication. Medication adherence was near optimal (80%) in the intervention month, but dropped off significantly (to 33%) when reminders and incentives stopped. While these initial results are promising, we need additional studies to assess true impact and what strategies we can use to diminish the sharp decline after the reminders and incentives are removed. Our team recently launched a randomized trial to answer these questions.
When it comes to care for underserved populations, there are several reasons why typical solutions may not deliver the same benefits seen in other populations. There may be:
- economic barriers to purchasing devices,
- difficulty establishing new routines in the presence of other competing family needs,
- greater barriers in establishing trust with providers and medication effectiveness,
- or a varying understanding of the consequences of asthma and appropriate asthma prevention.
All of these factors could contribute to lower levels of adherence to both provider recommendations and medication. With these barriers in mind, we must be thoughtful about the best ways to support and encourage families to modify long-standing behaviors that lead to low adherence. It is our hope that with continued research into how to couple the best behavioral science and evolving technology, we can help children like Michelle and her family improve their adherence to effective asthma medications, as we work toward broader solutions to reduce the asthma triggers in their homes, schools and communities.
*Name has been changed to protect patient identity
Chandler Floyd is a former clinical research assistant at PolicyLab.
Carina Flaherty is a former clinical research assistant at PolicyLab.
Kavya Sundar and Siobhan Costanzo, MPH, MED, former researchers at PolicyLab, contributed to this post.
