Tackling the Sexually Transmitted Infection Epidemic with Expedited Partner Therapy

Sexually transmitted infections (STIs) are at epidemic proportions in the United States, with unprecedented numbers of chlamydia and gonorrhea – 1.5 million and nearly 400,000 cases in 2015, respectively – reported by the Centers for Disease Control and Prevention (CDC). Adolescents and young adults ages 15-24 are disproportionately affected by these diseases, accounting for approximately two-thirds of chlamydia cases and one-half of gonorrhea cases. What’s more, up to 20 percent of young women are re-infected with these diseases within one year, most commonly due to lack of partner treatment, making screening and treatment crucial.
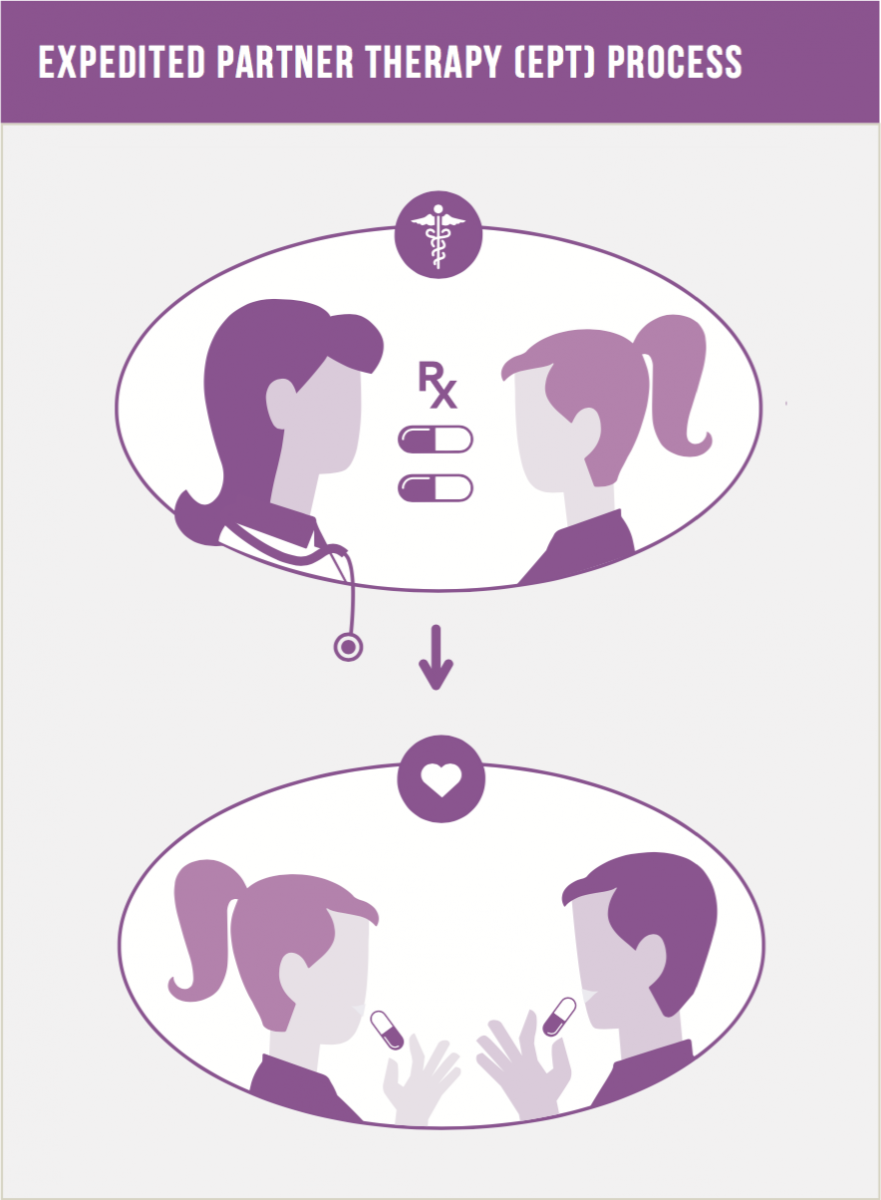
There are many potential solutions to tackling this epidemic including increased STI education among providers and the public, improved funding for clinics focusing on STI treatment and improved funding for health departments in order to facilitate identification and treatment of infected patients’ partners. One evidence-based approach to partner treatment is currently vastly underutilized – expedited partner therapy (EPT). With EPT, the medical provider gives a prescription or medication to a patient with chlamydia or gonorrhea to take to his or her partner. Multiple studies have demonstrated the effectiveness of this method in reducing reinfection rates, and jurisdictions across the country are utilizing EPT as one part of an STI reduction plan. However, given multiple policy and provider-based barriers, EPT use is not widespread.
As a pediatric emergency medicine provider, I am often confronted with caring for an adolescent diagnosed with an STI – and all too often, the encounter is not the patient’s first. Consider Nicole*, a 17-year-old who recently sought care in our emergency department for vaginal discharge. She was diagnosed with chlamydia, and treated with appropriate antibiotics; however, she confided in us her concern that she would be back again with similar symptoms within a few months. “I can’t get my [17-year-old] boyfriend John to the doctor – he says he’ll go, but then he says he never has time. I’ve already taken medicine for this twice in the last year!” With EPT, Nicole could take the medication or a prescription directly to John – eliminating his excuse of not having time to visit the doctor. While success in reducing STIs certainly requires more than EPT, this approach can make a significant difference.
However, depending on the state in which Nicole lives, the opportunity to utilize EPT varies considerably. For example, Rhode Island and Wisconsin have laws that explicitly allow physicians to prescribe EPT, Kentucky and West Virginia expressly prohibit EPT and multiple states have unclear regulations and potentially contradictory rules and laws.
As we describe in our new Evidence to Action brief, “Preventing Chlamydia and Gonorrhea Reinfection through Increased Use of Expedited Partner Therapy,” state medical boards and health departments can advocate for statutes and regulatory statements that more explicitly support the use of EPT, with the ultimate goal of consistency across states. The current inconsistency leads to provider confusion, particularly for those that practice in more than one state or have recently moved, which compounds other potential provider barriers to EPT implementation, such as concerns about medication delivery, missed opportunity of counseling of partners and the risk of adverse effects to the medication.
Without appropriate partner treatment, Nicole’s risk of reinfection is unacceptably high. She risks more significant infection, such as pelvic inflammatory disease, as well as chronic pain, infertility and increased risk for ectopic pregnancy, if her cycle of infection continues. While there are certainly other behavior changes that can impact reinfection, as providers we have the ability to provide medication to help ensure her long-term health. We need to work together to increase the use and availability of EPT as we work on multiple approaches to reduce the epidemic of STIs.
*This case is a composite of many and does not present identifying information of any single patient
