How Can We Improve LARC Access for Teens? Uphold ACA Mandates.
Imagine you are a pediatrician in the following scenario: a teen comes into your clinic two weeks after an episode of unprotected sex with her boyfriend. She took emergency contraception afterwards, and her pregnancy test is negative today in clinic. During this visit, she states that she is not ready to become pregnant and asks about her pregnancy prevention options. She expresses motivation to use the most effective form of contraception that is also reversible and will preserve her fertility. Together, you decide on a long-acting reversible contraceptive (LARC), and specifically an intrauterine device (IUD). Because you have to order the LARC to clinic, you make an appointment for her to return in two weeks. You know that due to the mandate by the Affordable Care Act (ACA), all preventive care, including contraception, is covered by insurance for all ages. However, the insurance company declines coverage of her IUD.
Is this a missed opportunity for the teen who is interested in contraception?
The United States continues to have a high rate of unintended pregnancy among teens despite some improvement in the past few years. In fact, the U.S. has among the highest teen pregnancy rates in the developed world. What opportunities are there to reduce this rate when young women come into clinics asking for contraception? Our recent research on insurance companies’ compliance with ACA mandates regarding contraception may highlight one of these opportunities.
While studies have examined health insurance plans’ compliance with the ACA mandate in adult health care settings, my recent research with Drs. Aletha Akers and Nadia Dowshen is the first study conducted in a pediatric health care setting. As adolescents have the highest rates of unplanned pregnancies, we sought to understand how insurers’ adoption of the ACA mandates could affect teens’ access to contraception.
Why is the ACA Important for Accessing LARCs?
The ACA ensured individuals could receive preventive care at no cost. This care encompasses coverage of all 18 U.S. Food and Drug Administration-approved contraceptive options, including LARCs. As with any new policy change, there were implementation challenges. Prior research shows that health care insurers have been inconsistent in complying with the ACA mandates. In fact, the issue of insurer adherence to the contraceptive coverage mandate in particular was so problematic that the federal government released a statement in Spring 2015 to reinforce that the ACA required contraceptive coverage without a co-pay.
We initiated our study in 2016, more than six years after the ACA was passed. Our team believed that this was ample time for hospital systems and insurers to adapt to the ACA requirements. As the study was initiated in the final year of President Obama’s second term, the ACA was not under threat in the same way that it was when he left office. We believe that this makes our results even more notable.
What Did We Want To Find Out?
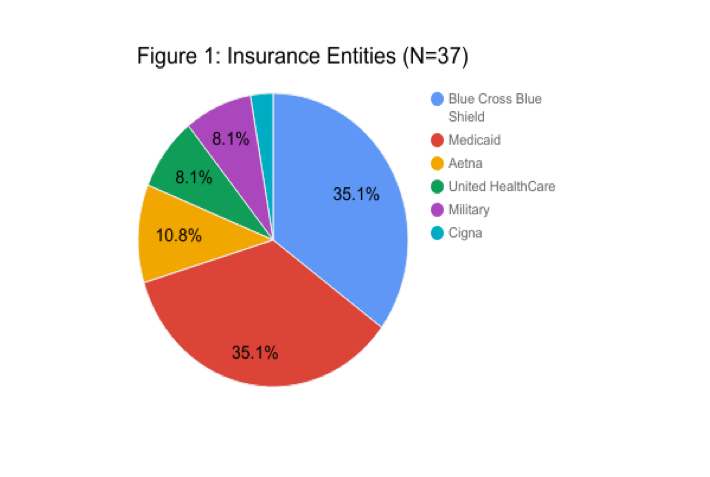
Our team had two main goals. First, we wanted to assess the adoption of the ACA’s contraceptive coverage mandates based on electronically available insurance resources in a pediatric health care system. Second, we sought to compare contraceptive coverage for Medicaid insurance plans and commercial plans. In our study, we included all 13 Pennsylvania Medicaid plans that cover patients seen at Children’s Hospital of Philadelphia and the 10 commercial plans with the largest market share.
We then utilized information from insurance plan websites including summaries of benefits and formularies. Two separate coders reviewed each plan’s information and categorized plans based on whether or not the insurance company covered each of the 18 contraceptive categories, and if the insurer considered the contraceptive method free preventive care or if they required a co-pay.
What Did We Learn?
Overall, we deemed 57% of insurance plans “adherent” because they stated they covered LARC services without a co-pay. Of the 43% of plans deemed “nonadherent,” three said they covered LARC services, but required a co-pay, whereas 13 did not cover LARC services at all. In addition, 94% of plans actually failed to adhere to the ACA mandate because they did not cover all 18 contraceptive categories. Finally, we learned there was no difference between private and public insurers.
What Are The Next Steps?
There are clear barriers to adolescent access to contraception, especially LARCs. One of these barriers is cost-sharing, or when a patient pays in the form of a co-pay or some other payment that their insurance company does not cover. While the ACA clearly mandates no cost-sharing for all 18 categories of FDA-approved contraceptives, many of the largest insurance companies we studied required cost-sharing.
Yet even in the best of circumstances, where LARCs are intended to be covered without cost-sharing, barriers remain. An adolescent seeking information online from a web-based insurance policy would likely not have success finding reliable, understandable information about plan coverage. This could interfere with them obtaining contraception, putting them at risk of experiencing an unintended pregnancy.
