Developing Sustainable Global Informatics Resources in Low-income Countries

Editor’s Note: This month, Children’s Hospital of Philadelphia will host the 13th Annual Pediatric Global Health Conference, during which participants can learn more about Global Health Informatics initiatives at CHOP, attend an informatics pre-conference session titled, “Designing Sustainable Global Informatics Resources in LMICs,” and more. Read about other topics that will be covered at the conference in a related blog post from members of CHOP’s Global Health Center.
Helping patients and their families live healthier lives is the ultimate goal for those in the health care profession. In much of the world today, health care workers achieve this goal by completing tasks that increasingly use health information technologies (health IT) such as the electronic health record (EHR). Health informatics is the field of work that blends together the people, tasks, and technologies necessary to improve the delivery of health care and, ultimately, health outcomes.
Ideally, health IT is introduced to augment, not replace or further burden, the work done by people in health care settings to make it easier to do the right thing for patients and their families. In global health, the goal of promoting healthier lives is the same, but the focus is on serving patients and their families living in resource-constrained settings, particularly those in low- and middle-income countries (LMIC). Joining these two fields, global health informatics applies health informatics approaches in resource-constrained settings.
Challenges to implementing health information technologies in LMICs
Health care workers in the U.S. and elsewhere who have survived any “go-live” health IT implementation have personal, sometimes painful, knowledge of the hurdles presented when these tools are introduced. Barriers common to all health care settings, whether low-, middle-, or high-income countries, include limited or no effort to build buy-in, resistance to change, limited experiences in technology and inadequate funding. Additionally, health IT implementation in LMICs faces unique challenges of unreliable electricity and internet infrastructures, lack of informatics training programs, and limited availability of commercial software that fit local health care needs and culture.
One barrier that continues to challenge the health informatics community globally is the ability to exchange and use data across different health IT software, also known as “interoperability.” When health IT is not interoperable, health care data is siloed in different software and cannot be automatically shared or used in any other systems. An example would be data on a child’s growth and immunizations being stored in a clinic’s EHR or health apps deployed on mobile phones (mHealth), but not easily shared with regional or national nutrition and immunization databases.
Without this shared data, health care workers across different clinics could face a daunting task of locating and treating malnourished or under-immunized children. The risk of costly duplication of effort is high in settings with already-limited human and financial resources. Multiply this problem by numerous disparate EHRs and mHealth apps introduced by various organizations across an entire nation and the challenge of sustaining such a system may seem insurmountable.
Innovative approaches to developing sustainable health information technologies
In global health, sustainability, mutual benefit and prevention of adverse impact are guiding principles for successful global child health partnerships. Similarly, global health informatics projects can avoid “pilotitis”—the failure of pilots to scale up—by prioritizing sustainability, scalability, interoperability and capacity-building. A partner-centered collaborative approach starts with understanding where the health care setting is on a digital health maturity scale. Health care settings in LMICs range from exclusive paper-based data entry, to transitioning to some digital data entry, to comprehensive national electronic health information systems.
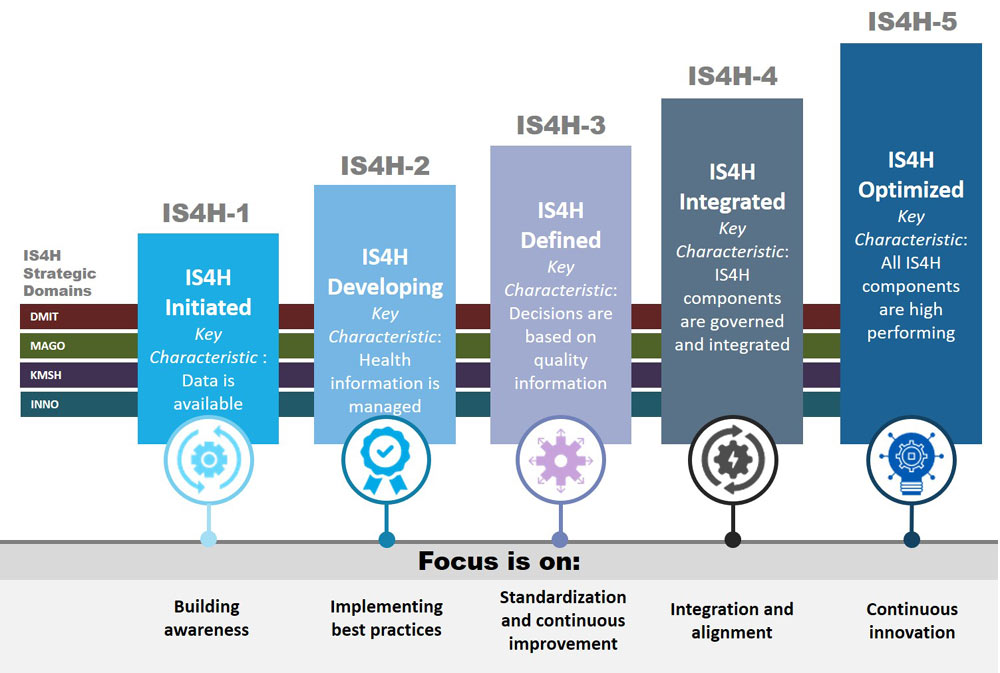
Figure 1. Digital Maturity Model, Pan American Health Organization (PAHO)
Based on the digital maturity level, health IT solutions can then be co-designed in partnership with local clinicians and experts to meet identified needs. As evidenced by the COVID-19 pandemic, the world is highly interconnected and these kinds of global health informatics collaborations are key to leveraging health IT to improve the quality of health for all.
How to be involved in global health informatics
For Informatics Professionals
U.S.-based informatics professionals can provide expertise through knowledge and skills exchange to support limited informatics expertise in LMICs. Health information system strategy and data warehouse optimization skills are much needed.
For Educators
Educators of all skill levels from informatics faculty, clinical informatics champions and informatics trainees (fellows, residents) can all participate in workforce development in LMICs where informatics training opportunities are limited.
For Researchers
Researchers collecting or analyzing data in settings outside the U.S. can apply global health informatics principles of sustainability, scalability, and capacity-building using universal messaging standards and open source tools, partnering with local clinical workers to ensure that the tools augment, and do not burden, patient care.
For Individual Clinicians
Individual clinicians practicing in the U.S. can advocate, lead, and participate in patient-facing quality improvement or operational projects that prioritize health IT solutions for newcomers, refugees, migrants and patients for whom English is a second language.
For Policy-focused Professionals
Leaders can amplify global health informatics as a priority within state, federal and international informatics professional communities. For example, robust leadership is needed to strengthen collaborations with international informatics bodies such as the International Medical Informatics Association, WHO and UNICEF. Advocating for funds to be allocated to improve the quality of care and health outcomes globally could support informatics research, training, and capacity in low- and middle-income country institutions in partnership with U.S. institutions and investigators. Decision-makers can also show support for a concerted digital health equity plan for local global health informatics, prioritizing EHR interventions to improve the health of newcomer, refugee, immigrant and migrant populations living in the U.S. Finally, advocacy is needed for the development of standards that govern simple, accessible, multilingual digital health resources.
Anyone who provides health care to these communities through the use of health IT is practicing global health informatics. Those who design and implement the tools used are also practicing global health informatics. Global health informatics principles can be applied both in the U.S. and beyond to advance sustainable, scalable and capacity-building health IT design that achieves the ultimate goal of better health for all.
Bernard Caines is an IT specialist and data analyst for Niños Primeros en Salud in Consuelo, Dominican Republic.
Sansanee Craig, MD, is an assistant professor, clinical informaticist and co-chair of the newly established Global Health Informatics Unit at CHOP.
Grey Faulkenberry, MD, MPH, is a clinical informaticist and co-chair of the newly established Global Health Informatics Unit at CHOP.
Anthony Luberti, MD, is the medical director of informatics education in the Department of Biomedical and Health Informatics at CHOP.
Kagiso Ndlovu, MSc, is a computer scientist and eHealth research unit coordinator at the University of Botswana.
