Black Breastfeeding Matters: Mitigating Racial Inequities in Child Health Outcomes
Breastfeeding/chestfeeding has numerous well-described short- and long-term health benefits for infants and caregivers. A recent survey of breastfeeding in Philadelphia, however, highlighted disparities in lactation that have long been known. Despite lactation initiation prevalence being at or above 80% within all races individually, 79% of White parents reported any breastfeeding at eight weeks postpartum, as compared to 59% of Black parents and 58% of Hispanic/Latinx parents. This data suggests the presence of racial and ethnic disparities in lactation duration. Though this inequity is increasingly receiving recognition, as seen with the revised 2022 American Academy of Pediatrics (AAP) Breastfeeding Policy, it nonetheless requires further attention as to identify the root cause(s) and potential solution(s) to improve health outcomes among the most vulnerable communities.
Breastfeeding has evolved into more of a privilege than a right, particularly in the wake of recent formula shortages. This is, in part, due to fragmented health care systems and suboptimal policies for parental leave and support. As a pediatrician practicing in West Philadelphia, many of the families I see express a clear desire to breastfeed their infants, yet they struggle to reach their personal goals. The reasons behind lactation cessation are multifold, but frequently relate to a lack of access to personal and professional lactation support, as well as the need to return to work. A 2018 survey in Philadelphia reported insufficient milk supply and difficulty with latch as the most frequent reasons for lactation cessation among Black participants, both challenges that could be addressed with improved access to professional lactation support.
Philadelphia has the highest infant mortality rate in the United States. Mortality rates among Black infants are consistently higher than rates among all other racial and ethnic groups (see graph below). This disparity is unfortunately not isolated to Philadelphia: mortality rates among Black infants are highest across races nationwide. These children deserve the attention of clinicians, policymakers and health systems at large to improve their outcomes. Increasing breastfeeding has the potential to help mitigate this unacceptable inequity.
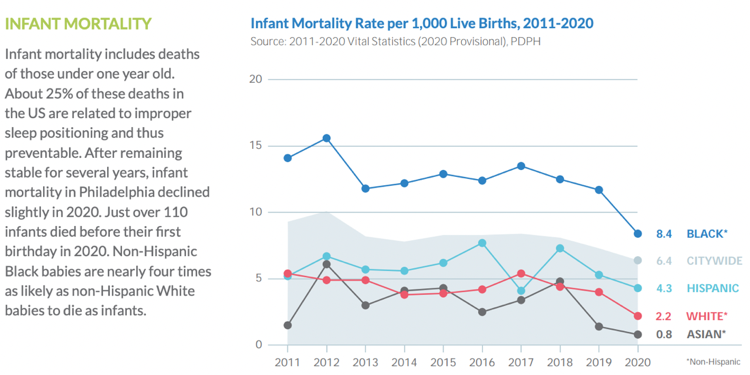
Source: City of Philadelphia’s Department of Public Health’s 2021 Health of the City report
Getting the Word Out Into the Community
To help address barriers faced by Philadelphia’s families in achieving their infant feeding goals, I collaborated with local filmmakers, parents, and community organizations to create a short three-part film series aimed at 1) outlining the impact of racism on lactation rates within the Black community; 2) providing accessible patient education on the benefits of breastfeeding; and 3) highlighting community-based lactation resources currently available to families within the prenatal, perinatal and postnatal periods. I invite you to view and share this series with those whom you feel would benefit from its content.
Addressing racial and ethnic disparities in lactation demands policies that facilitate lactation initiation and duration, particularly for parents of racial/ethnic minority backgrounds. Health systems and policymakers must place value in and partner with Black, Indigenous, and Latinx patients, researchers, organizations, and health care professionals to design and implement policies that support lactation.
5 Ways to Support Philadelphia’s Families with Breast/Chestfeeding
1) Funding should be allocated to build and support programs that provide professional training to Black and Brown individuals who wish to become lactation specialists. More specifically, individuals could be reimbursed for becoming board-certified lactation consultants or peer counselors within their community. Alternatively, public insurance could improve coverage of and reimbursement for postpartum lactation services to incentivize this as a career option. Investing in racially concordant care could also help build a sizable and sustainable network of culturally informed, trusted community-based lactation support, harnessing the experience and wisdom that already exists within the community.
2) Health systems should require that all health care professionals interacting with prenatal and postpartum families achieve minimum competency in providing breastfeeding education and basic hands-on support to birthing individuals and their infants, particularly those experiencing barriers to reaching their feeding goals. This may include trainings on the management of common lactation challenges and trauma-informed care.
3) Local, state, and federal lactation policies should be centered around a reproductive justice framework aimed at supporting all Black and Brown birthing individuals. For example, policies that incentivize—or better yet require—employers to provide protected space and time to pump (ideally outside of scheduled breaks and lunch times) are critical for those working in non-office settings. This is particularly true for individuals working in the service and transportation industries where these protections are not routinely guaranteed. Additionally, public payers could subsidize or cover the cost of hands-free pumps to support those parents with less flexibility and privacy in the workplace.
4) Public health officials must work to normalize and provide public examples of Black breastfeeding, for example, through billboards, public ads and social media campaigns featuring Black families breastfeeding.
5) Hospitals that largely care for marginalized communities should be strongly incentivized to achieve and maintain their Baby Friendly designation in order to optimize breastfeeding support and minimize formula use unless personally preferred or medically necessary.
Call to Action for Health Care Professionals
By helping families reach their personal infant feeding goals and improving lactation duration—particularly within the Black community—potential exists to decrease both infant mortality rates and the incidence of diseases that disproportionately impact children of color. This includes conditions such as asthma, obesity and type 2 diabetes. Providing culturally sensitive breastfeeding support is a seemingly simple intervention with large promise, impacting the individual, greater communities and health systems at large. Clinicians, public health officials, and policymakers must not miss this opportunity to improve health equity and work to close some of the many gaps observed in maternal and child health outcomes.
Deanna Nardella, MD, is a recent graduate of Children's Hospital of Philadelphia’s Pediatrics Residency Program and a current postdoctoral fellow within the National Clinician Scholars Program at Yale University. She recommends “Magical Milk,” a children’s book written by a Philadelphia-based lactation specialist working to normalize breastfeeding at an early age and improve representation.
