The Message Matters: Exploring Parent and Provider Priorities for Child Wellness

Child wellness involves not only physical health, but mental, social and educational well-being. It also includes characteristics of family and community environments that support healthy growth and development. However, less than one-third of U.S. children experience physical, psychological, social, and educational well-being, and two-thirds face challenges related to their family, neighborhood or socioeconomic circumstances. To reverse these negative trends and help children achieve optimal wellness, health promotion in early childhood is crucial.
The pediatric primary care office is a trusted source of information on child health and well-being and is particularly well-suited to help families promote wellness. The American Academy of Pediatrics even developed recommendations to help guide these discussions. However, studies show that visit time restrictions and heavy workloads are barriers for providers to addressing all recommended health promotion topics in pediatric primary care.
For example, at the four recommended preventive visits for children between the ages of 2 and 4, professional guidelines advise that they receive screenings for nine developmental and behavioral health assessments alone. This does not include various other screenings, assessments and conversations that occur at these time-constrained visits. To help providers prioritize wellness topics for discussion during pediatric primary care visits, we designed a study to understand parents’ and clinicians’ priorities for wellness in early childhood, and to look at how they align and differ from one another.
Understanding Where Parents & Providers Stand on Importance of Wellness Topics
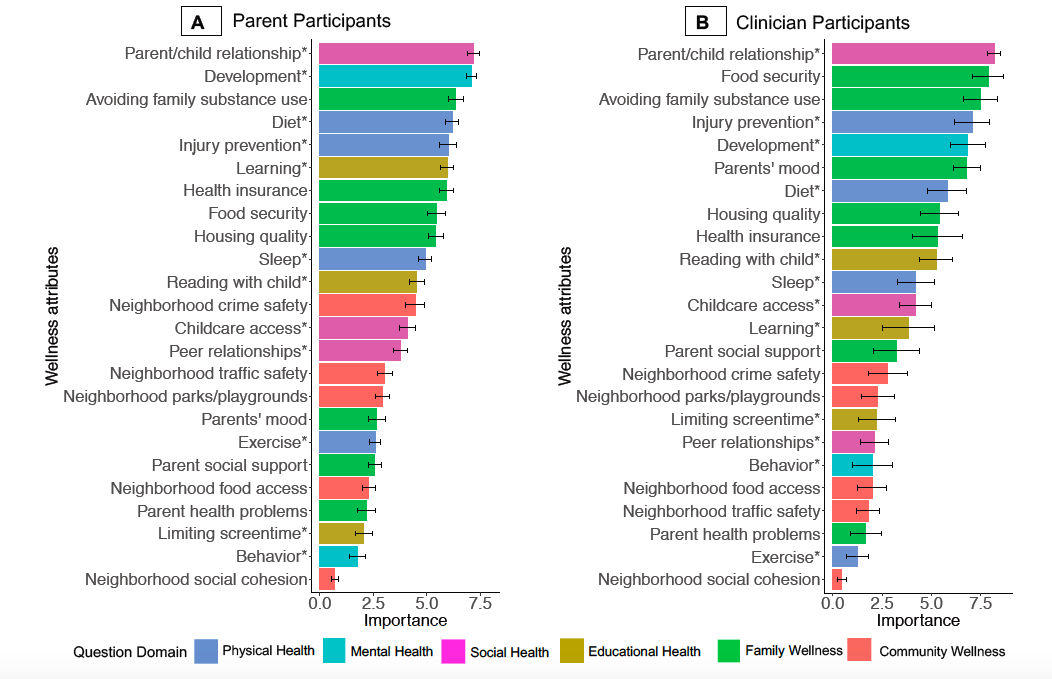
We found that child-level and family-level wellness attributes ranked higher for both parents and clinicians than community-level wellness attributes. Both parents and clinicians highly prioritized the parent-child relationship and avoiding family substance use. Parents more strongly prioritized child learning while clinicians more strongly prioritized food security and parent mood (for example, whether a parent is experiencing depression or anxiety symptoms). Both groups ranked social connections between neighbors and parent health problems lower compared to other wellness items. (See graphic below.)
First published in the Journal of Child and Family Studies, Vol. 30, pages 2238–2249 (2021) by Springer Nature
Understanding these priorities is important because if recommended screenings and subsequent conversations and guidance provided by clinicians are not resonating with parents, then the screening itself could be of low value for their child’s health. Therefore, identifying wellness topics that can be reframed to resonate more strongly with parents may help to maximize wellness promotion opportunities in pediatric primary care.
Reframing Conversations to Meet Parent Priorities
Screen time
One topic that was not highly prioritized by parents was limiting screen time. However, we know that screen time has been linked to both obesity and future chronic disease in children, so finding a way to reframe this topic could be key to long-term child health. Instead of discussing the unfavorable impacts of screen time with parents of young children, clinicians could reframe the conversation to emphasize the importance of high-quality screen time. For example, web-based applications or educational programs can support child learning and parent-child interactions, topics that parents ranked as highly important.
Parent health problems and parent mood
Parent health problems and parent mood were also not highly prioritized by parents; while clinicians did not highly prioritize parent health problems, they did identify parent mood as an important wellness factor for young children. Parent physical and mental health is shown to influence child health outcomes, and parents’ mood has been shown to influence the parent-child relationship and child development, items which parents prioritized very highly.
These conversations can be difficult to address in pediatric health care settings, as parents likely expect the focus of the visit to be on their child. However, developing intergenerational family services to provide parents with resources and support for their own mental health at pediatric visits could be critical to supporting child health outcomes that parents find very important.
Food security
Food security is another item that clinicians ranked as very important while parents prioritized other wellness topics. Screening families for food security in the pediatric health care settings is recommended, but screening itself is not enough. Once a family has been identified as food insecure, additional steps must be taken to provide the family with resources.
It is important to note that food security has been found to be associated with child development and learning, which parents prioritized more strongly. If a family does screen positive for food insecurity, a clinician could provide resources while also giving the family an understanding of the positive impacts that those resources could have on their child’s development and learning.
Community support
Finally, neighborhood social cohesion was ranked as less important by both parents and clinicians. Addressing neighborhood relationships and community support is not traditionally addressed in primary care, so clinicians could consider not addressing this topic during well visits to allow for prioritization of issues that both parents and clinicians resonate with more strongly.
Ensuring that topics important to parents are addressed in pediatric primary care is crucial to improving child health outcomes. However, topics that are important to wellness but less highly prioritized by parents may require reframing to focus on links with wellness topics parents do find important. Such reframing could be a way to address topics that parents have less interest in or are more sensitive to discuss, ensuring that children still receive early interventions and guidance from clinicians, while also being respectful and responsive to parental priorities. In future research, our team will look more closely at family characteristics to understand similarities and differences among families when considering wellness to help further enhance and tailor opportunities to support child health in primary care settings.
Chloe Hannan, MS, is a former clinical research coordinator at PolicyLab.
