Improving Health Care One Community at a Time
Editor’s note: This is part of our social determinants of health blog post series, which features content from PolicyLab experts and guest authors. We invite you to check back in for new posts, read the last post in the series, or follow along for updates on Twitter at @PolicyLabCHOP.
For a myriad of social and economic factors, the United States is experiencing growing disparities in health outcomes and a declining average life expectancy. We’re also paying more than any other country for this tragic trend—$3.6 trillion annually on health care or $11,172 per person. To turn the tide on our ratio of dollars spent to life span will require radical changes to health care norms. Addressing social determinants of health (SDOH) is vital to creating a new paradigm and fundamentally improving the drivers of health.
In Utah, we are taking an executive-supported, grassroots-implemented approach to improve health one community at a time. The Alliance for the Determinants of Health is a three-year demonstration modeled after the Center for Medicare & Medicaid Services’ (CMS) Accountable Health Communities Model of awareness, assistance and alignment. Two counties are piloting this model among a segment of the state’s Medicaid population. Our chief aims are to identify sharable and scalable best practices, reduce health care costs and improve overall well-being. In this piece, I will highlight how we are implementing each piece of the model.
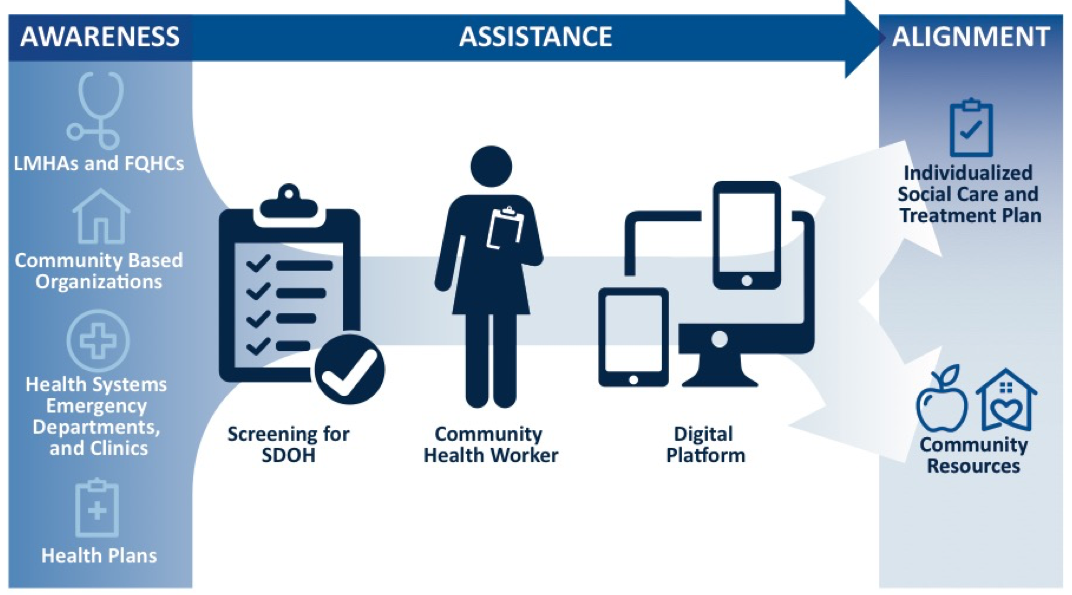
Building Awareness Through a “No Wrong Door” Approach
The Alliance is organized and convened by Intermountain Healthcare and its health plan, SelectHealth. Intermountain provided a $12 million community contribution to support the work; however, from the on-set we designed the Alliance to be a community-led collaborative. Taking a “no wrong door” approach to engage SelectHealth Medicaid members, a cross-section of community organizations conduct evidence-based SDOH screenings and coordinate health care, behavioral health and social services for Alliance participants.
The community organizations gear these SDOH screenings toward members identified through claims data with high emergency department utilization for non-emergent conditions. The Alliance provides lists of these high utilizers by attribution to Federally Qualified Health Centers (FQHCs), local mental health authorities and Intermountain clinics. Then, SelectHealth care managers proactively reach out to members for screening, particularly those not attributed to a primary care physician (PCP). Additionally, alerts built into Intermountain’s electronic health record notify emergency departments and behavioral health urgent care centers when these members are admitted to the hospital.
Participants are connected directly to community services by the provider when social need is identified during screening, or with the support of an Alliance community health worker (CHW) who is employed by an independent community-based organization, the Association for Utah Community Health. This support could range from sharing information about nearby food banks to more complex situations like securing housing and finding specialty care.
The network of organizations providing and connecting participants to services are working through a shared technology. Using a web-based platform powered by Unite Us, organizations can securely coordinate care between health care and social services. It also provides a shared bucket for SDOH data collection that can identify gaps in community resources.
Bridging the Cultural Gap
The Alliance CHWs play a unique role in bridging the cultural gap from participant to provider, as well as provider to provider. CHWs are a mobile team working within the walls of various community organizations and have the flexibility to conduct home visits. The secret sauce CHWs bring to the mix is their advocacy for participants, which garners trust and empowers people to take incremental steps toward larger change. The CHWs have unique lived experience that allows them to relate to barriers participants face. Likewise, their expertise alleviates the apprehension some clinical providers have in screening for SDOH. Thus, CHWs become a trusted ally for providers and help mitigate the burden of care management teams.
CHWs meet with participants one-on-one to conduct in-depth SDOH assessments and use motivational interviewing to guide the participant’s prioritization of next steps. The CHWs also have discretionary funds to assist with one-time costs that are not covered by Medicaid or other community organizations. Costs are often under $200, but can be a game changer. For example, one CHW provided a participant with a taxi voucher from the county jail to a homeless shelter, which helped ensure his road to sobriety. He told the CHW that without the coordinated support, his next call was to his circle of substance-using associates. This individual is now 10 months sober.
Coming Together to Improve Care
The Alliance also convenes care coordination meetings between organizations screening for SDOH, CHWs and SelectHealth to provide updates on shared cases. Giving everyone around the table the ability to communicate and work collectively has been key to success. These meetings provide insight into participants’ care—ranging from scheduling transportation to accessing specialty care—and allow teams to share notes and eliminate duplicative efforts. It also is a forum to strategize how and where to find the hardest-to-reach members.
In one instance, a CHW assisted a Spanish-speaking mother and her 8-year-old son with Down syndrome with navigating a language barrier between health care providers and school staff. The school sent home a recommendation for speech therapy, but mom was unable to understand the communication. Coordinating with the PCP, the CHW assisted the family during a well-child check to express a need for specialty care referrals. The CHW supported the family in scheduling appointments for speech, occupational and behavioral therapy. The CHW also connected the mother to an ESL class and a community organization that provides free specialized respite care.
Identifying Best Practices
The net goal of the Alliance demonstration is to create a model for sustainable SDOH practices to implement system-wide and share nationally. To that end, PolicyLab is partnering with the Alliance to assess participants’ experiences, how it impacts their overall well-being and how the interventions affect health care costs. In collaboration, PolicyLab will also conduct a policy analysis to understand best practices for developing, garnering funding for and scaling up an intervention such as the Alliance. Combined, this information should produce a useful roadmap for other health systems considering interventions in the area of SDOH.
Amber Rich is a Community Partnership Specialist for the Alliance for the Determinants of Health.
