Improving Equitable Identification of Developmental Delays and Autism Spectrum Disorder
Statement of Problem
According to the Centers for Disease Control and Prevention, an estimated 1 in 59 children have autism spectrum disorder (ASD). Despite the high prevalence, significant disparities exist in identifying ASD and other developmental disabilities in young children from ethnic/racial minority backgrounds, as well as girls. Early identification of ASD, which allows for the earliest possible intervention, helps children to be their healthiest selves, yet children of color and girls are more likely to be identified at later ages—if at all. They are also under-represented in early intervention (EI) services—including speech/language therapy, occupational therapy and special education—for developmental delays. In turn, these disparities in identification and access to services can prevent vulnerable populations from receiving necessary autism-specific interventions.
Description
Improving Equitable Identification of Developmental Delays and Autism Spectrum Disorder
Improving Equitable Identification of Developmental Delays and Autism Spectrum Disorder
Pediatricians were more likely to refer children who are white, male and from an English-only speaking home. These findings suggest that differences in referrals may impact children’s access to diagnostic and intervention services and may contribute to disparities in ASD diagnosis.
Pediatricians are tasked with discussing developmental concerns with caregivers (known as developmental surveillance) and with screening children for developmental delays and ASD at specified doctor’s visits using standardized screening tools. The goal of this body of research is to determine if the process of surveillance and screening may contribute to disparities in ASD identification, and if we can modify this process to promote equity in detection and referral for intervention.
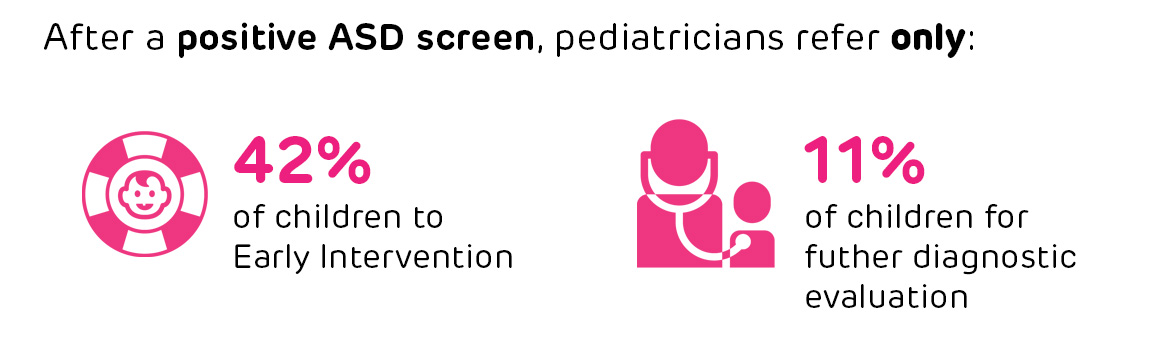
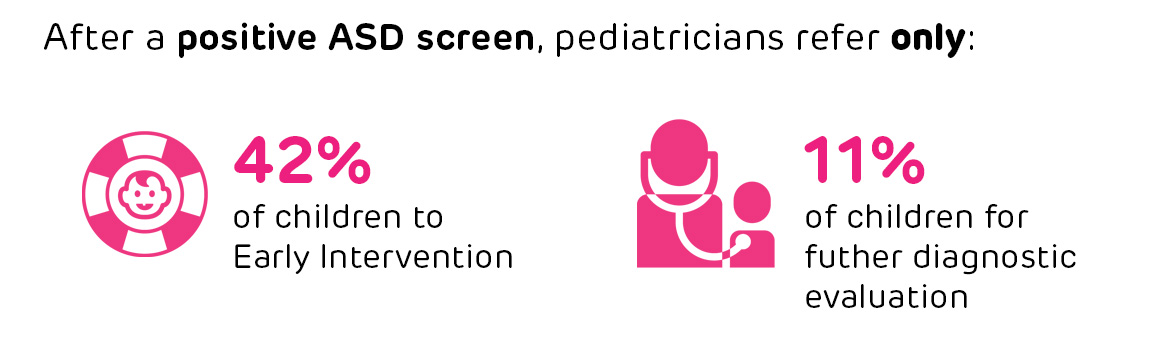
First, Dr. Wallis and her team examined pediatricians’ adherence to guidelines for referral to services after a young child screens positive for ASD. Using data from the electronic health record, the researchers found that pediatricians refer 42% of children to EI after a positive ASD screen, but only 11% for a further diagnostic evaluation, as guidelines ask them to do. Additionally, they are more likely to refer children to EI who are white, male and from an English-only speaking home. These findings suggest that differences in referrals after a positive screen may impact children’s access to diagnostic and intervention services and may contribute to disparities in ASD diagnosis. There is room for improvement for all children to access evaluations after a positive screen.
Through that work, Dr. Wallis also noted that pediatricians referred about one-fourth of children to EI even before their positive ASD screen, which suggests that some children have developmental concerns identified very early and can benefit from services at a young age. She also found that children who are white, Hispanic or from an English-only speaking home are more likely to be involved with EI prior to a positive ASD screen. These findings emphasize that early initiation of EI may be related to disparities in ASD identification.
To further explore the identification process of ASD and developmental disabilities in pediatric primary care, Dr. Wallis sought to understand how doctors and caregivers discuss how a child is meeting developmental milestones and learning new things. Asking caregivers about any concerns in regards to how the child is developing is part of the process of developmental surveillance. She collected audio recordings of pediatricians and caregivers during well-child visits for young children between 15 and 36 months. After analyzing these recordings using a standardized coding scheme—the Roter Interaction Analysis System—the researchers found that all well-child visits included some discussion of development. Few parents asked developmental questions, but they were willing to provide information about their child’s development. These findings suggest there are areas for improvement to engage parents in these discussions.
Next, Dr. Wallis and her team decided to run similar analyses to evaluate which children pediatricians referred early to EI, prior to screening positive on a general developmental screen or on the day of a positive developmental screen. Using data from the electronic health record, Dr. Wallis found that children who pediatricians referred early—even before the screen took place—were more likely to be white and male, or have public insurance. Children who pediatricians referred to EI on the day of the positive developmental screen were more likely to be black versus white and have a lower household income. These findings suggest that screening may aid in identifying and referring children who otherwise may not have had access to EI services at a young age.
Dr. Wallis has two additional studies that are related to this body of work:
- Dr. Wallis collaborated with Children’s Hospital of Philadelphia’s Center for Autism Research to conduct the first real-world study on universal screening for ASD. They found that the M-CHAT/F, a widely-used screening tool, is less accurate than previously shown for identifying children with ASD, especially those who are non-white, lower income and from non-English speaking homes, but is still a valuable tool.
- Dr. Wallis contributed to a systematic review that focused on the availability, translation and cultural validation of screening instruments to detect developmental concerns in U.S.-based Hispanic populations. The findings suggest that translation into Spanish alone is insufficient, as there may be cultural differences that impact the validity of screening between non-Hispanic and Hispanic populations, which can impact how pediatricians identify developmental issues in children with Spanish-speaking families.
Next Steps
Through these various studies, Dr. Wallis and her team are gaining an understanding of the processes that may be contributing to disparities in ASD identification among children of color, low-income children and girls. While we have known for many years that ethnic/racial minority and low-income populations and girls are more likely to be diagnosed with ASD at later ages, if at all, these studies inform our understanding of some of the mechanisms by which delayed identification occurs.
Dr. Wallis aims to use these insights to develop strategies for bettering the process of developmental surveillance and screening, improving developmental outcomes for all children, and bridging gaps in identification and care for low-income and ethnic/racial minority children and girls with developmental delays and ASD.
This project page was last updated in March 2020.
Suggested Citation
Children's Hospital of Philadelphia, PolicyLab. Improving Equitable Identification of Developmental Delays and Autism Spectrum Disorder [Online]. Available at: http://www.policylab.chop.edu. [Accessed: plug in date accessed here].