Medicaid’s Role in Supporting Youth with Disabilities Into and Through Adulthood

Erin* is a young woman in her late 20s. She works two jobs, and in her free time she enjoys going to the gym and spending time with friends, some of whom she has remained in touch with since high school. She pays rent on her apartment and has no trouble covering her bills and expenses with her earnings.
Erin also has both physical and intellectual disabilities. She uses a wheelchair, and requires assistance with all aspects of her care, including eating and using the bathroom.
Impact of Community Supports
With appropriate supports, individuals with intellectual and developmental disabilities (IDD) like Erin have the capacity to participate in their communities, enjoy recreational activities with family and friends, and often maintain competitive employment. Until the age of 21, supports for people with IDD are primarily provided through special education services in the school system and through Medicaid’s Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) program. As outlined in our recent Evidence to Action brief and policy brief on transitioning to adult care, EPSDT provides services — such as home nursing and physical and occupational therapies that assist with functioning — that allows individuals with IDD to go to work, socialize and maintain a lifestyle that mirrors the able-bodied adults around them.

After age 21, young adults with IDD graduate from high school and lose eligibility for EPSDT. The loss of services can place significant stress on parents and other caregivers whose daytime support for their adult children with IDD may take priority over working their own full- or part-time jobs. For caregivers facing their own health care challenges, the problem is further exacerbated. Erin’s mother, Felicia*, who participated in our research study about long-term care planning for adults with IDD, has a chronic illness herself and thus cannot provide most of the physical support that Erin needs on a daily basis.
Impact of Medicaid
Fortunately, Erin is eligible for services through Medicaid’s Home and Community Based Services (HCBS) waiver. Because of this program, she successfully maintains her active lifestyle and lives in her own apartment. The waivers cover personal and attendant care services that assist people with IDD and other disabilities with tasks such as eating, bathing, dressing, preparing meals, and going grocery shopping. They also cover habilitative services that help people with disabilities learn independent living skills; assistive technology, such as lifts, wheelchairs, and speech-generating devices; and supportive housing services.
Without staff support, funded through the HCBS Medicaid waiver, Felicia and Erin would be forced to pay exorbitant amounts of money out-of-pocket for the services that allow Erin to maintain an active lifestyle. If she didn’t have access to these services, Erin could not work and would need to live in an institution. This result would be a great loss for Erin, as well as her family and friends, and it would be a significantly greater expense for taxpayers.
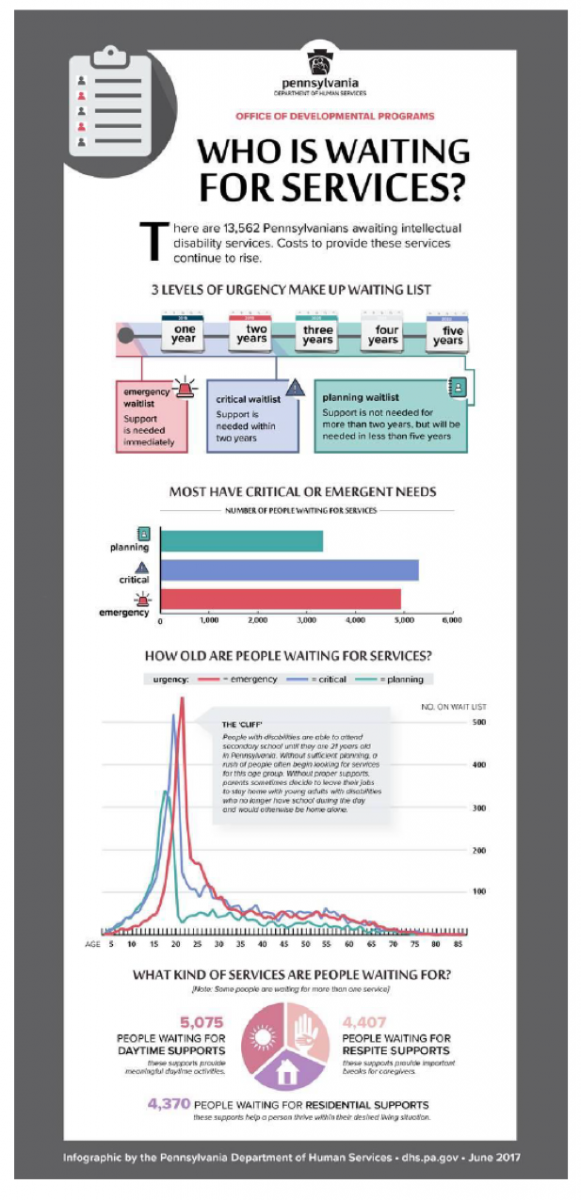
While HCBS waiver funding can successfully support adults with IDD and help them continue to live in their homes and communities, the long waiting list for these services can delay access for years in some cases. In Pennsylvania alone, the waiting list includes more than 13,500 individuals. The highest number of those needing emergent services, meaning that the individual’s health and safety is at risk if they do not receive services immediately, are young adults in their 20s who have just stopped receiving school and EPSDT services.
Fortunately, some policymakers have noticed the issue and taken steps to resolve it. In his recently passed 2017-2018 state budget, Pennsylvania Governor Tom Wolf allocated $26.5 million toward services for individuals with IDD, including reducing the waiting list by 1,000 people, providing funding for 820 new graduates of special education programs, and developing two new hospital units to support the medical and behavioral health needs of individuals with IDD. While the budget is not yet funded, this allocation has the potential to reduce stress and greatly improve the lives of thousands of individuals living with IDD and their families.
Conversely, recent proposals to reduce federal Medicaid funding could devastate adults with IDD and their caregivers. Medicaid is the primary payer for long-term services and supports for individuals with disabilities, and plays a key role in helping states finance services to meet their community integration obligations under the Americans with Disabilities Act and the Supreme Court’s Olmstead decision, which found that unjustified institutionalization of people with disabilities as illegal and discriminatory.
Though we are not sure what the future of health care reform looks like, we can be certain of how proposed policies would likely impact people from this vulnerable population. Proposals to cap and cut Medicaid would likely lead to a reduction in HCBS funding, as these are optional for states, leading to longer waiting lists for services and requiring more individuals with IDD to enter institutions to receive care.
Maintaining funding for Medicaid is critical in helping to ensure that the most vulnerable young adults in our country have the supports and services to lead healthy and productive lives after high school graduation. For young adults with IDD, Medicaid funding is not just a safety net program, it is the mechanism which allows them to contribute to their communities and to the economy. While Governor Wolf is working hard to ensure that Pennsylvania's adults with IDD and their families have the supports that they need, federal cuts to Medicaid could detrimentally alter the day-to-day livelihood of individuals and families like Erin and Felicia.
*Names and some details have been changed to protect patient and family privacy
Sophie Jan and Caren Steinway are former PolicyLab researchers who continue to collaborate with our center on various projects related to youth with complex medical needs and transitioning from pediatric to adult care.